Valley Fever Cases Spike in California – What You Need to Know

Valley fever, also known as coccidioidomycosis, has become a pressing health issue in California, as highlighted by recent reports from state health officials. In 2023 alone, there have been 6,761 confirmed cases of this fungal infection, a number that could escalate dramatically if current trends continue. This illness is caused by inhaling spores from the Coccidioides fungus, which thrives in California’s soil, particularly after periods of drought followed by rain. The symptoms of Valley fever can mimic those of other respiratory ailments, making early diagnosis crucial for effective Valley fever treatment. As public health authorities warn of rising incidence rates, it is essential for Californians to be aware of the dangers and recognize the symptoms associated with this increasingly common illness.
Often referred to as coccidioidomycosis, Valley fever is an infection caused by a soil-dwelling fungus that flourishes in specific regions of the United States, especially California. This particular illness poses an escalating concern for residents in areas like the San Joaquin Valley, where cases are surging year after year. The spores released into the air can lead to various health challenges, often initially mistaken for common colds or flu-like symptoms. As California health officials grapple with rising numbers of infections, understanding the potential risks and symptoms becomes increasingly important. Being informed about Valley fever symptoms and treatment options can empower individuals, especially those within high-risk categories, to seek timely medical attention.
Understanding Valley Fever: What You Need to Know
Valley fever, also known as coccidioidomycosis, is primarily caused by inhaling spores from the Coccidioides fungus found in soil, particularly in the San Joaquin Valley of California. This infection has gained significant attention due to a troubling spike in cases reported throughout California. Health officials note that as of July, there were nearly 7,000 confirmed infections, a number indicating a concerning trend that could see annual totals reaching unprecedented heights in the coming years. The rise of Valley fever cases is directly linked to environmental conditions that favor the growth of the Coccidioides fungus, particularly periods of drought followed by rainfall.
The California Department of Public Health (CDPH) has been closely monitoring this situation and raising public awareness about the seriousness of Valley fever. As moisture levels fluctuate, the fungus becomes more active, leading to increased exposure for individuals in high-risk areas. Furthermore, with the possibility of climate change influencing weather patterns, experts are predicting that valley fever cases could continue to rise in the state. It is crucial for residents in affected areas to educate themselves on how to prevent infections and recognize the symptoms.
Symptoms of Valley Fever: Identifying the Signs
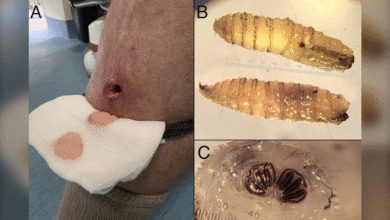
The symptoms of Valley fever can mimic other respiratory illnesses, which complicates early diagnosis. Commonly reported symptoms include fever, chills, fatigue, chest pain, joint pain, and severe headaches. In some cases, especially among those with compromised immune systems, Valley fever can escalate to more severe complications such as meningitis, necessitating immediate medical attention. The variability of symptoms means that vigilance is necessary; one should not dismiss early signs as merely a seasonal flu or cold. As Dr. George Thompson pointed out, the clinical presentations can be quite diverse, making it imperative for individuals living in endemic areas to undergo testing if they suspect exposure.
Early detection is critical, especially considering the potential long-term implications of untreated Valley fever. Symptoms can linger and lead to protracted health issues, including severe pulmonary problems requiring hospitalization. For individuals aged 60 and above, pregnant women, and those living with chronic health conditions, the stakes are even higher. Understanding and recognizing these symptoms early can play a vital role in effective treatment and recovery.
The Rise of Valley Fever Cases in California
California is facing an alarming increase in Valley fever cases, with confirmed reports nearing 7,000 as of mid-2023. This remarkable uptick is raising concerns among health officials, as it could be part of a broader trend influenced by climatic factors and changing environmental conditions. The California Department of Public Health has indicated that the numbers are likely to rise due to delays in reporting and ongoing environmental challenges that favor the spread of the Coccidioides fungus.
According to experts, the steady rise in Valley fever cases over the past few years is not merely a statistical fluctuation but rather a reflection of shifting ecological conditions that could worsen in the future. Dr. Thompson noted that there is a correlation between increased outdoor activities in dusty environments and the incidence of Valley fever, particularly among those involved in construction, gardening, or archaeological projects. For California residents, staying informed about the potential risks is essential.
Valley Fever Treatment Options: What You Should Know
Effective treatment for Valley fever largely depends on the severity of the illness and the patient’s overall health. Mild infections may resolve on their own, but for those experiencing significant symptoms or for higher-risk populations, antifungal medications such as fluconazole are commonly prescribed. Understanding that Valley fever can cause serious complications is vital for patients, particularly those with weakened immune systems. Treatments can last from several weeks to months based on the patient’s response.
For individuals recovering from severe cases, ongoing management and follow-up medical care might be necessary. This extended care is essential to address potential complications that can arise from the infection, such as chronic respiratory issues or the progression of the disease beyond the lungs. As cases of Valley fever increase, it’s imperative that patients work closely with healthcare providers to monitor their symptoms and adjust treatment plans as needed.
Prevention Strategies for Valley Fever
Preventing Valley fever primarily involves minimizing exposure to the Coccidioides fungus, especially in areas where it is known to thrive. California residents are encouraged to avoid activities such as digging in the soil or spending prolonged time in dusty environments, particularly during dry months. Wearing protective equipment, such as N95 masks, can significantly reduce the risk of inhaling fungal spores, especially during dusty conditions or construction activities.
Health officials emphasize that awareness and education are key in prevention efforts. Understanding when and where Valley fever is most likely to occur can help individuals take proactive measures to protect themselves. Public health campaigns focused on reducing exposure risks and informing communities about Valley fever can ultimately lead to lower case numbers, safeguarding the health of those living in affected regions.
High-Risk Groups for Valley Fever
Certain populations are at a higher risk of developing severe illness from Valley fever, including individuals over the age of 60, those with compromised immune systems, and people with underlying health conditions such as diabetes. Furthermore, ethnic groups, specifically those identified as Black or Filipino, may have increased vulnerability to the disease. Health officials stress the importance of targeted communication regarding the risks faced by these individuals so that they can take appropriate precautions and seek medical advice promptly if symptoms arise.
Understanding the demographic factors that contribute to the risk of Valley fever is essential for effective community health planning. Tailored approaches to education and prevention can help safeguard at-risk groups and promote early detection and treatment, minimizing the impact of the disease on these vulnerable populations. Engaging with healthcare providers about individual risk factors and the latest guidelines can empower at-risk individuals to better manage their health.
The Environmental Impact on Valley Fever Incidence
The relationship between environmental conditions and the incidence of Valley fever is becoming increasingly clear. Studies have shown that the Coccidioides fungus flourishes in drought conditions, followed by rainfall, which releases spores into the air. These spores can easily become airborne, increasing the likelihood of inhalation by individuals nearby. California’s changing climate poses new challenges as these conditions may become more frequent, thereby raising the overall risk of Valley fever.
Community awareness regarding environmental factors is essential in combating the rise of Valley fever cases. Actions such as dust control at construction sites, public education initiatives concerning soil disturbance, and climate resilience planning can help mitigate the risks associated with Valley fever. By addressing the root causes of environmental change, California can work towards reducing the incidence of this serious illness.
Seeking Medical Care for Valley Fever Symptoms
If you suspect you have been exposed to Valley fever or are experiencing concerning symptoms, it is crucial to seek medical attention promptly. Healthcare providers are equipped to perform tests that can confirm a diagnosis of Valley fever, allowing for timely intervention. Early diagnosis can significantly affect outcomes and help prevent complications. Symptoms such as persistent fever, chest pain, and difficulty breathing should never be ignored, particularly in individuals belonging to high-risk groups.
Discussing your symptoms and exposure history with your healthcare provider can foster better understanding and treatment plans. Valley fever is manageable, especially with early intervention, and open communication is key to achieving the best health outcomes. Regular follow-ups may also be necessary for those diagnosed with Valley fever to monitor recovery and prevent any potential complications from arising.
Valley Fever Awareness and Community Action
Increasing awareness of Valley fever within communities is vital to controlling its spread. Community health initiatives focusing on education about the disease, its transmission, and prevention strategies can empower residents to take proactive steps in reducing their risk. Local health officials and organizations play a crucial role in disseminating information and resources to enhance public understanding of Valley fever.
Additionally, fostering community discussions about the environmental factors that contribute to the rise in Valley fever cases, such as soil management practices and regional development, can lead to collective action. Engaged communities advocating for preventive measures, such as dust suppression in urban areas, can make a significant difference in controlling the incidence of Valley fever, ultimately protecting public health.
Frequently Asked Questions
What are the common Valley fever symptoms to watch for?
Common symptoms of Valley fever include fever, chills, fatigue, chest pain, and night sweats. Other symptoms may involve joint pain, weight loss, severe headaches, and skin rashes. If you experience symptoms resembling a respiratory infection, particularly after visiting areas with known Coccidioides fungus, it’s important to seek medical advice.
How are Valley fever cases trending in California currently?
As of July 2023, California health officials reported a significant rise in Valley fever cases, with 6,761 confirmed cases. The trend indicates that cases may exceed the previous record of 12,595 set in 2024, raising concerns about the ongoing impact of Valley fever within the state.
What is the Coccidioides fungus and how does it relate to Valley fever?
The Coccidioides fungus is the causative agent of Valley fever, an infection contracted through inhaling fungal spores found in the soil, particularly in areas like the San Joaquin Valley, Southern Arizona, and parts of California. Awareness of this fungus is essential for understanding how to minimize exposure and the risk of infection.
What treatment options are available for Valley fever?
Valley fever treatment typically involves antifungal medications. For severe cases, hospitalization may be necessary. Ongoing medical care is crucial for those experiencing persistent symptoms or complications from Valley fever, such as severe respiratory issues or meningitis.
Who is most at risk for Valley fever according to California health officials?
Certain groups are particularly at risk for Valley fever, including individuals aged 60 and older, those with compromised immune systems, pregnant women, and individuals with diabetes or certain ethnic backgrounds like Black or Filipino. Understanding these risk factors is key to prevention.
Are there effective prevention strategies for Valley fever?
Yes, effective prevention strategies for Valley fever include avoiding dusty areas or construction sites where soil is disturbed and wearing N95 respirators in high-risk environments. Staying informed about local conditions that may promote Coccidioides fungus growth can also help.
How can exposure to Valley fever be minimized in California?
To minimize exposure to Valley fever in California, avoid outdoor activities in dusty environments during high winds or after rainstorms. Additionally, be cautious when engaging in hobbies that disturb the soil, and consider using protective masks, such as N95 respirators.
What long-term effects can Valley fever have on individuals?
Long-term effects of Valley fever can include chronic respiratory issues and the potential for the infection to spread to other parts of the body, including meningitis in 1% to 3% of cases. Continuous medical care may be required for those who experience severe complications.
Is Valley fever disease confined only to California or found elsewhere?
While California has a high prevalence of Valley fever, especially in Southern California and the San Joaquin Valley, the disease is also commonly reported in Arizona, New Mexico, Utah, Texas, Nevada, and parts of Washington State. This highlights the need for awareness across these regions.
What measures do health officials recommend for those living in Valley fever-prone areas?
Health officials recommend that individuals living in Valley fever-prone areas be aware of the symptoms and risk factors associated with the disease. They should take preventive measures like avoiding construction sites, wearing masks in dusty conditions, and regularly checking for updates on local disease activity.
| Key Point | Details |
|---|---|
| Current Cases | As of July 2023, California reported 6,761 confirmed cases of Valley fever. |
| Historical Data | Valley fever cases in California averaged between 7,000 and 9,000 annually from 2016 to 2024. |
| Future Projections | If trends continue, cases for 2025 could exceed 12,595. |
| High-Risk Groups | Individuals at increased risk include: those over 60, immunocompromised people, pregnant women, and those with diabetes. |
| Symptoms | Symptoms may include fever, chills, fatigue, respiratory issues, and severe cases may involve meningitis. |
| Prevention Tips | Avoiding dusty environments, wearing N95 masks, and steering clear of disturbed soil areas can help prevent infection. |
Summary
Valley fever cases are rising sharply in California, with health officials noting a significant increase in confirmed infections. As awareness of this serious disease grows, understanding its symptoms, risks, and preventive measures becomes crucial. By sharing knowledge and proper precautions, Californians can help combat the spread of Valley fever.