Transorbital Approach: A Breakthrough in Spinal Tumor Surgery
The transorbital approach represents a groundbreaking advancement in spinal tumor surgery, showcased in a recent innovative procedure performed at the University of Maryland Medical Center. Surgeons successfully navigated through a patient’s eye socket to remove a chordoma, a rare spinal tumor, thus transforming the landscape of neurosurgery in Maryland. This remarkable technique not only allows direct access to tumors that were previously deemed inoperable but also minimizes external scarring, making it a significant achievement in surgical innovation. For young patients like Karla Flores, the transorbital approach offers a lifeline by enhancing surgical options and reducing the risk of complications. As researchers and surgeons continue to explore its potential, this novel technique could pave the way for future breakthroughs in the treatment of spinal tumors.
The transorbital approach, often referred to as eye socket surgery, is reshaping the methodologies employed in neurosurgery by providing innovative access points for tumor removal. This technique allows surgeons to approach tumors located near the spine through the eye socket, drastically improving safety and efficacy while addressing complex cases like chordomas. By employing a minimally invasive strategy, this method not only transforms the way spinal tumors are surgically addressed but also highlights the evolution of techniques in spinal tumor surgery. Surgeons are now better equipped to manage challenging cases, ensuring that patients experience less trauma and better recovery outcomes. As the medical community embraces this approach, it is positioned to revolutionize treatments for spinal tumors and enhance patient care.
Understanding Chordomas: A Rare Spinal Tumor
Chordomas are a rare type of tumor that arises from the cells of the spine, particularly affecting the vertebrae. Characterized by their slow growth, they can occur at the base of the skull or along the spinal column. Despite being relatively uncommon, with approximately 300 new cases diagnosed annually in the United States, chordomas pose significant health risks due to their invasive nature and proximity to critical neurological structures. The complexity of treating such tumors often leads to challenges in surgical management, highlighting the importance of advanced surgical techniques in neurosurgery.
These tumors typically arise from remnants of the notochord, which is a structure present during embryonic development. Patients diagnosed with chordomas may experience a variety of symptoms depending on the tumor’s location. In many instances, they can present with severe pain, neurological deficits, and in some cases, symptoms related to vision, as seen in the case of Karla Flores. Surgical innovation in approaches to chordoma removal is vital, as traditional methods may not be feasible due to the tumor’s location and growth patterns.
The Revolutionary Transorbital Approach in Neurosurgery
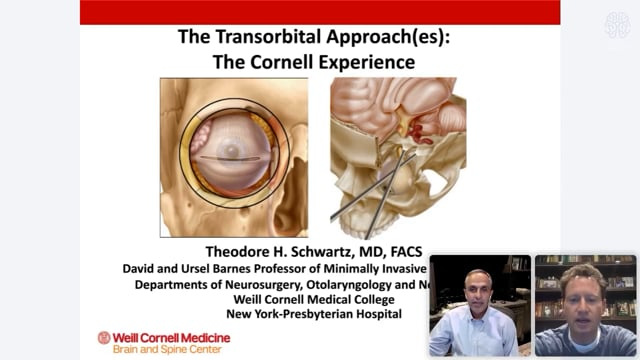
The transorbital approach is a novel surgical technique that allows neurosurgeons to access tumors located around the spinal cord via the eye socket. This minimally invasive method offers surgeons a direct and unobstructed path to reach difficult-to-access tumors that were previously considered high-risk due to their proximity to vital structures. The ingenuity behind this surgical innovation not only improves visibility during surgery but also significantly minimizes the risk of damaging critical nerves and blood vessels, thus reducing the chances of complications such as paralysis or speech difficulties.
During the recent groundbreaking surgery on Karla Flores, a surgical team at the University of Maryland Medical Center successfully utilized the transorbital approach to remove her chordoma. By strategically navigating through the eye socket, they created a surgical corridor that bypassed conventional routes laden with risks, showcasing the potential for this method to revolutionize spinal tumor surgery. As Dr. Mohamed Labib articulated, the transorbital approach provides a ‘straight shot’ to the tumor, which significantly enhances the precision of the procedure and the overall outcomes for patients.
Challenges and Risks in Spinal Tumor Surgery
Surgical interventions for spinal tumors, particularly chordomas, are fraught with challenges and inherent risks. Neurosurgeons must navigate a complex anatomy that includes critical neurological structures like the spinal cord, brainstem, and major blood vessels. In the case of chordomas, the tumor’s location can complicate removal, as seen in the case of the young Maryland woman, where the tumor had integrated with her spinal anatomy. Despite meticulous planning and advanced surgical techniques, the threat of complications such as damage to the brainstem or spinal cord looms large.
The potential consequences of surgical missteps not only include immediate risks associated with the surgical procedure but also long-term outcomes for patients. For instance, uncontrolled growth of chordomas can lead to debilitating symptoms and significantly impact the patient’s quality of life. Therefore, the evolution of surgical methods, such as the transorbital approach, represents a critical advancement in neurosurgery that seeks to mitigate these risks while effectively addressing the tumor.
Post-Surgical Recovery and Rehabilitation
Post-operative recovery for patients like Karla Flores is crucial in the overall treatment of chordomas. Following her innovative transorbital surgery, Flores began her journey towards recovery, emphasizing the need for patient resilience and proper rehabilitation. The complexity of her operation necessitated careful management of her recovery process, including monitoring for potential complications and adjusting to any changes resulting from the surgery. Key components of her recovery included rest, physical therapy, and psychosocial support to cope with the emotional facets of her diagnosis.
Moreover, the multidisciplinary approach undertaken by the surgical team ensured that Flores received comprehensive care post-surgery. Pain management, nutritional support, and regular follow-ups are integral aspects of recovery that can significantly aid a patient’s return to normalcy. As highlighted by Dr. Labib, fostering a supportive environment enables patients to focus on rehabilitation, paving the way for successful reintegration into daily life and contributing to an optimistic prognosis.
The Role of Multidisciplinary Teams in Tumor Treatment
The treatment of complex spinal tumors like chordomas often requires a multidisciplinary approach involving a diverse team of specialists. Neurosurgeons, orthopedic surgeons, radiologists, and rehabilitation experts must collaborate to devise a comprehensive treatment strategy aimed at addressing both the tumor and the associated challenges of recovery. This collaborative effort not only enhances surgical outcomes but is essential in planning post-operative care, ensuring that all aspects of the patient’s health are considered.
In Karla Flores’ case, the integrated care model enabled seamless communication among various specialists, including facial plastic surgeons and oncologists, highlighting how innovative surgical techniques, like the transorbital approach, complement the need for a cohesive treatment plan. The synergy between different specialties enhances the likelihood of success, reduces recurrence rates, and improves overall patient satisfaction by providing holistic and patient-centered care.
Advancements in Cancer Treatment: Innovations in Surgery
Technological advancements have significantly transformed surgical practices and cancer treatment in recent years. Innovative techniques and tools, such as image-guided surgery and minimally invasive approaches, are now integral to the management of complex tumors. As with the novel transorbital approach utilized in the removal of Karla Flores’ chordoma, these innovations not only aim to improve surgical precision but also enhance recovery times and minimize complications.
Moreover, as surgical innovations continue to evolve, the opportunities for improving outcomes in spinal tumor surgery become more promising. The focus is shifting towards preserving surrounding healthy tissues while achieving complete tumor removal, ultimately leading to better long-term prognoses for patients. The continued development of such cutting-edge techniques represents a beacon of hope for patients diagnosed with challenging tumors, allowing for enhanced quality of life post-treatment.
The Importance of Early Diagnosis in Tumor Management
Early diagnosis of spinal tumors, including chordomas, plays a pivotal role in effective management and treatment. Symptoms such as double vision, pain, or neurological deficits often serve as critical warning signs; however, these symptoms can sometimes be misattributed to other conditions. In the case of Karla Flores, her experience with double vision ultimately led to the timely identification of her chordoma. Prompt recognition of these indicators is fundamental in improving patient outcomes and curtailing tumor progression.
Research emphasizes that the earlier a tumor is diagnosed and treated, the greater the chances of successful intervention and recovery. Health education regarding the signs and symptoms associated with spinal tumors is vital, as it empowers patients to seek medical attention sooner. Comprehensive approaches focusing not only on treatment but also on awareness can significantly enhance survival rates and overall quality of life for individuals faced with these daunting diagnoses.
Future Directions in Neurosurgery and Tumor Treatment
The future of neurosurgery and tumor treatment is poised for remarkable advancements, especially with the introduction of innovative surgical methods like the transorbital approach. The University of Maryland Medical Center’s team plans to showcase this technique to neurosurgeons globally, highlighting its potential to revolutionize how challenging tumors are addressed. As the medical community embraces these innovations, training and knowledge dissemination will be essential in broadening the reach of such techniques to benefit patients everywhere.
Furthermore, ongoing research aimed at understanding the mechanisms behind chordomas and other spinal tumors is crucial in paving the way for novel therapeutic options. As new insights emerge, there is hope for even more targeted treatments that not only focus on surgical intervention but also incorporate advanced modalities such as immunotherapy and targeted therapies. The integration of multidisciplinary efforts in research and surgical practices promises an exciting future for patients battling these formidable tumors.
Patient Empowerment and Education in Cancer Care
Patient empowerment plays a crucial role in navigating the complexities of cancer care. Educating patients about their diagnosis and treatment options, as well as involving them in the decision-making process, fosters a sense of agency and hope. For individuals like Karla Flores, receiving comprehensive information about her chordoma and the surgical approach that would be taken laid the foundation for informed consent and active participation in her care.
Incorporating educational resources in patient care not only aids individuals in understanding the medical terminologies and processes involved but also equips them with the knowledge to seek support and advocate for their needs. Needing to understand their diagnosis can alleviate anxiety and foster resilience, as patients embark on their treatment journeys equipped with the confidence to engage in their healthcare decisions.
Frequently Asked Questions
What is the transorbital approach in spinal tumor surgery?
The transorbital approach is a novel surgical technique used to access the spinal cord through the eye socket, specifically developed to remove spinal tumors like chordomas. This method allows surgeons to create a direct pathway to the spine while minimizing damage to surrounding structures.
How does the transorbital approach improve outcomes for patients with chordoma?
This innovative approach improves outcomes for chordoma patients by providing a less invasive way to access tumors wrapped around the spinal cord. By utilizing the eye socket, surgeons can reduce risks associated with traditional approaches, leading to quicker recovery times and fewer complications.
What are the risks associated with the transorbital approach when treating spinal tumors?
While the transorbital approach minimizes external scarring and damage to critical structures, risks include potential injury to the brainstem, spinal cord, or blood vessels. Surgeons meticulously plan and practice the procedure to mitigate these risks, particularly in complex cases involving chordoma.
Is the transorbital approach commonly used in neurosurgery for spinal tumors?
The transorbital approach is a relatively new surgical innovation in neurosurgery, specifically for spinal tumors. It was first utilized at the University of Maryland Medical Center, showcasing its potential as an alternative for challenging cases that require alternative access routes.
How does the transorbital approach enhance surgical precision in spinal tumor surgeries?
This technique enhances surgical precision by allowing a ‘straight shot’ access to the spinal cord through the lower eye socket, which helps surgeons effectively remove spinal tumors like chordomas while minimizing the need to navigate through complex anatomical structures.
What kind of training do surgeons undergo before utilizing the transorbital approach?
Surgeons, such as those involved in the transorbital approach for spinal tumor surgeries, typically undergo extensive training, including practicing the procedure on cadavers multiple times to ensure they are well-prepared for the intricacies involved in operations involving delicate structures.
Can the transorbital approach be used for other types of tumors beyond chordomas?
While primarily developed for chordomas, the transorbital approach may have applications for other types of tumors located near the spinal cord and brain, demonstrating versatility in neurosurgery. Continued research and clinical trials will likely expand its use.
What is the recovery process like after a transorbital surgery for spinal tumors?
Recovery after a transorbital surgery for spinal tumors varies by patient, but many, like Karla Flores, experience positive outcomes, including reduced pain and a quicker return to daily activities. Close follow-up care and individualized rehabilitation plans are crucial for a successful recovery.
How has the transorbital approach been presented in the context of global surgical practices?
The transorbital approach has garnered international attention, with UMMC planning to demonstrate the technique at their annual Skull Base surgery course. This presentation aims to share knowledge and expand the adoption of this innovative approach among neurosurgeons worldwide.
What are the future implications of the transorbital approach in neurosurgery?
The future implications of the transorbital approach in neurosurgery include the potential for broader applications in treating spinal and brain tumors, reducing cancer recurrence rates, and improving patient outcomes, paving the way for more innovative surgical practices.
| Key Point | Details |
|---|---|
| Patient Background | Karla Flores, 19, diagnosed with a chordoma, a rare bone tumor affecting the spine. |
| Surgery Overview | Novel transorbital approach used to remove tumors wrapped around spinal cord through the eye socket. |
| Risks Involved | High risk of paralysis or death if major structures like spinal cord or brainstem were injured during the procedure. |
| Surgical Team | Dr. Mohamed Labib (neurosurgeon) collaborated with Dr. Kalpesh Vakharia (facial plastic surgeon) to ensure minimal external scarring. |
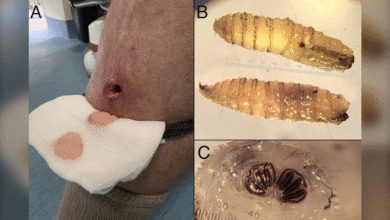
| Reconstruction | Post-tumor removal, the eye socket was reconstructed with a titanium plate and hip bone. |
| Recovery and Future Plans | Flores is recovering well and plans to return to school. Further demonstrations of the transorbital surgery will occur globally. |
Summary
The transorbital approach has emerged as a groundbreaking technique for spinal tumor removal, minimizing risks and improving patient outcomes significantly. In the case of Karla Flores, this innovative method allowed for the successful extraction of her chordoma through her eye socket, a first in medical practice. The collaborative effort of the surgical team not only focused on tumor removal but also on aesthetic considerations, ensuring a scar-free recovery. As more surgeons learn this technique, it has the potential to revolutionize how similar conditions are treated, offering hope to many patients facing life-threatening tumors.