Sperm Donor Genetic Mutation Linked to Cancer Cases
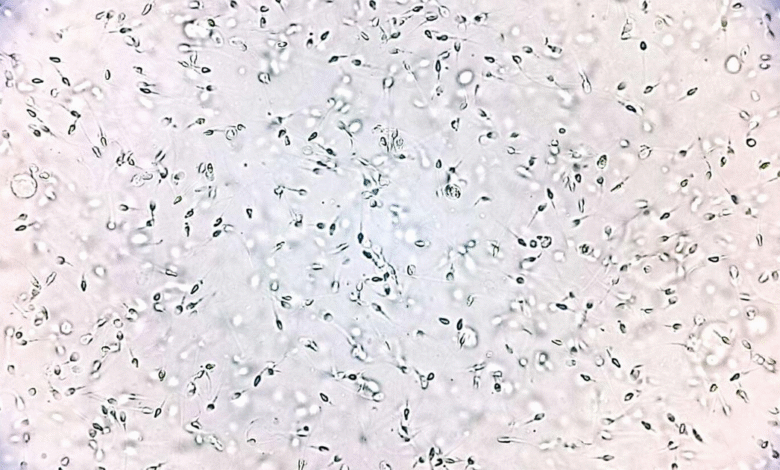
The topic of sperm donor genetic mutation has gained prominence following troubling revelations linking a single sperm donor in Europe to multiple cancer cases among offspring. Recent reports indicate that sperm donated by this individual, who carries a rare TP53 mutation, has been used to conceive at least 67 children, with 10 diagnosed with various types of cancer, including leukemia. These alarming statistics raise serious questions about current sperm donor screening procedures and the effectiveness of existing sperm donation guidelines. As experts push for stricter regulations, the case highlights the need for enhanced genetic screening to identify potentially harmful genetic variants associated with conditions like Li-Fraumeni syndrome, which significantly elevates cancer risk. This incident underscores the urgent requirement for families considering sperm donation to thoroughly understand the implications of genetic mutations and the safeguards that should be in place.
Exploring the implications of genetic variants in sperm donations, the concept of sperm donor hereditary mutations is critical, especially given recent findings that underline the connection between certain mutations and serious health risks. The case that has emerged involves a sperm donor with a mutation in the TP53 gene, known for its link to cancer, raising red flags about reproductive assistance and the health of conceived children. As discussions around sperm donor genetic screening evolve, alternative terms like semen donor genetic variations and hereditary risks in sperm donation are becoming increasingly relevant. Addressing these genetic concerns is essential for prospective parents seeking donor sperm while ensuring rigorous adherence to sperm donation regulations and safeguards. Such precautions are vital not only for the health of future generations but also for reinforcing trust in reproductive health practices.
Understanding Sperm Donor Genetic Mutations and Cancer Risks
Sperm donor genetic mutations have been increasingly scrutinized in light of recent findings linking certain genetic variants to an elevated cancer risk in children conceived through assisted reproductive technologies. Notably, a specific mutation in the TP53 gene, responsible for the proper regulation of cell division and tumor suppression, has been identified as a risk factor that contributes to Li-Fraumeni syndrome. Parents should be aware that this syndrome raises the likelihood of developing cancers such as leukemia and various sarcomas at a significantly younger age. Understanding these genetic implications is essential for families considering sperm donation.
The discovery of this genetic mutation serves as a critical reminder of the importance of genetic screening and counseling in sperm donation processes. The issue was thrust into the spotlight when reports emerged about 10 children affected by cancer linked to sperm from a single donor with the TP53 mutation. This scenario not only emphasizes the potential consequences of genetic risks but also highlights the need for stringent guidelines and screening protocols within fertility clinics and sperm banks to mitigate such risks and prevent tragic outcomes.
Sperm Donor Screening Practices and Their Limitations
Current sperm donor screening practices in the U.S. are guided by recommendations from the American Society for Reproductive Medicine (ASRM) and regulations mandated by the FDA. While these guidelines include comprehensive health assessments and genetic screenings, they may not be enough to unveil all potential genetic mutations that could pose health risks to offspring. Specifically, the standard practices do not include whole-genome sequencing, which could identify rare but consequential mutations like TP53 that link to serious conditions such as cancer.
Moreover, the adherence to donor limits varies significantly across regions, which can lead to potential overuse of specific donors, increasing the risk of genetic disorders in children. As illustrated by the case in Europe where a donor fathered 67 children, all donors should ideally have caps on the number of families they can contribute to in order to minimize the spread of genetic diseases, including those linked to sperm donor genetic mutations. These challenges highlight the necessity for continuous improvements in donor screening methods and establishing international guidelines to protect future generations.
The Impact of Li-Fraumeni Syndrome in Children Conceived via Sperm Donation
Li-Fraumeni syndrome is a hereditary condition that greatly increases the risk of developing multiple cancers during a person’s lifetime, often at a young age. For children conceived using sperm donors carrying the TP53 mutation linked to Li-Fraumeni syndrome, the implications can be dire. Reports indicate that out of 67 children born to one donor, 10 faced cancer diagnoses, which underscores the urgent need for thorough genetic assessments. Parents who have children through sperm donation must consider genetic counseling to understand their child’s risks and implications fully.
The troubling outcomes associated with Li-Fraumeni syndrome spotlight the necessity for sperm banks to revise their screening protocols to include more targeted genetic tests for known cancer-associated mutations. Educational initiatives should also be launched for prospective parents about the potential repercussions of genetic mutations carried by sperm donors. This awareness would empower families to make informed decisions about sperm donation and its consequences for their children’s health.
Exploring the Role of Sperm Donation Guidelines in Preventing Genetic Complications
The sperm donation landscape is influenced by a myriad of guidelines aimed at safeguarding the health of conceived children. The American Society for Reproductive Medicine recommends limiting the number of births per sperm donor to reduce the risk of genetic complications among offspring. For instance, the ASRM suggests a maximum of 25 live births per donor in populations of up to 800,000. Such measures are intended to prevent genetic diseases from disproportionately affecting children conceived through generous donors.
With revelations regarding the TP53 mutation in sperm donors, these guidelines may require a reevaluation to include more advanced genetic screenings that can anticipate rare but serious genetic risks. Each sperm donor possesses a unique genetic makeup that must be carefully assessed to avoid unintended health consequences for prospective families. Future modifications to sperm donation guidelines must incorporate the latest findings and technologies to ensure safer reproductive practices.
Sperm Donor Genetic Counseling: Why It Matters
Genetic counseling plays a critical role in the sperm donation process, particularly in light of alarming findings related to genetic mutations that could pose significant health risks. Parents considering using a sperm donor should seek genetic counseling to inform themselves about potential risks associated with specific genetic mutations, such as the TP53 variant linked to Li-Fraumeni syndrome. Understanding these genetic risks can equip parents with the necessary knowledge to make informed decisions regarding family planning and to seek appropriate medical support for their children.
Additionally, genetic counseling can facilitate discussions about the importance of long-term health monitoring for children conceived through sperm donation. In cases where fathers may have contributed genetic material connected to increased cancer risk, ongoing medical oversight becomes essential. Genetic counselors can guide families through the complex implications of genetic inheritance and provide tailored support based on each family’s unique circumstances, ultimately aiming to improve health outcomes for children.
The Need for Enhanced Genetic Screening in Sperm Banks
The evolving landscape of genetic research necessitates a reevaluation of the screening practices adopted by sperm banks worldwide. The case of the European sperm donor with the TP53 mutation serves as a cautionary tale about the inadequacies of current screening methods, which often do not capture rare but impactful genetic variants. Enhanced genetic testing protocols should be developed and implemented, potentially incorporating whole exome or whole-genome sequencing to identify hazardous mutations before a donor’s sperm is used.
Additionally, stricter regulations may need to be instituted globally to require comprehensive genetic history evaluations for sperm donors. By doing so, sperm banks can significantly reduce the risk of transmitting harmful genetic conditions to offspring. This proactive approach to genetic screening and regulation could play a crucial role in preventing cases similar to those that recently emerged, where multiple children with cancers were affected by a single donor’s genetic mutation.
Challenges in Sperm Donation Regulations Across Different Countries
Regulations governing sperm donation vary widely across different countries, leading to inconsistencies in how genetic risks are managed. For example, while the European Sperm Bank has introduced its own family limits for sperm donors, in the U.S., there is no stringent legal cap, leaving more room for the potential spread of genetic mutations. This disparity creates challenges in ensuring the safety of donor-assisted reproduction across borders, especially as more couples seek international sperm donation options.
Furthermore, discrepancies in genetic screening practices mean that donors who may pose risks due to unrecognized mutations could be responsible for conceiving numerous children. As shown by the incident involving the TP53 mutation, this can lead to unexpected and tragic health implications for the children conceived. As such, collaboration between international entities to harmonize sperm donation regulations and genetic screening practices is urgently needed to protect the health of future generations.
Recommendations for Parents Considering Sperm Donation
For parents contemplating sperm donation, understanding the genetic risks associated with potential donors is paramount. It is crucial to engage in open discussions with reproductive specialists about the screening protocols employed by sperm banks and whether they include testing for known genetic mutations, such as those related to cancer predispositions. Seeking detailed information about the donor’s medical history and ensuring access to genetic counseling can offer families essential insights regarding their reproductive choices.
Moreover, parents should be proactive about pursuing genetic testing for their children, especially if conceived through sperm donors with any known genetic concerns. Early intervention can greatly aid in managing potential health risks, providing peace of mind, and enabling families to plan for their children’s futures. Ultimately, taking informed steps in the realm of sperm donation can help families navigate the complexities surrounding genetic inheritance.
The Future of Sperm Donation and Genetic Screening
Looking towards the future, the field of sperm donation is poised for significant advancements in genetic screening and regulation. With ongoing research revealing the profound implications of genetic mutations like the TP53 variant in sperm donors, it is imperative that sperm banks adapt their practices to prioritize the health and safety of offspring. Implementing cutting-edge genetic tests and establishing international guidelines will become increasingly crucial in mitigating the risks associated with genetic disorders.
As society becomes more aware of the pivotal role genetics play in health, both parents and sperm banks must collaborate to foster an environment of transparency and safety. This partnership will not only contribute to better reproductive outcomes but also ensure that families have the necessary support and information to navigate their unique journeys through sperm donation and genetic health management.
Frequently Asked Questions
What is the impact of a sperm donor genetic mutation like TP53 on cancer risk for offspring?
The TP53 mutation is linked to Li-Fraumeni syndrome, which significantly raises the risk of developing cancer. Children conceived from sperm donors with this genetic mutation may face a higher likelihood of cancer diagnoses, as evidenced by cases where 10 out of 67 children from a single donor developed cancer linked to this mutation.
How does sperm donor screening prevent genetic mutations like Li-Fraumeni syndrome?
Sperm donor screening aims to identify known genetic mutations and health issues that could affect offspring. In the case of the TP53 mutation associated with Li-Fraumeni syndrome, standard screening methods failed to detect this genetic variant at the time of donation, highlighting the limitations of current sperm donation guidelines in preventing genetic risks.
What should parents do if their child is conceived by a sperm donor with a known genetic mutation?
If a child is conceived through a sperm donor carrying a genetic mutation, such as TP53, it’s crucial for the family to seek genetic counseling. This can help assess the potential health risks associated with the genetic mutation and provide information on monitoring and preventive measures.
What are the sperm donation guidelines regarding genetic screening for inherited mutations?
Sperm donation guidelines typically require comprehensive health screenings, including family medical history and infectious disease testing. However, as seen with the TP53 mutation, some genetic mutations may go undetected due to the limitations of standard screening practices, indicating a need for updated guidelines to encompass more robust genetic evaluations.
How can the risk of cancer in children from sperm donors be mitigated according to current research?
Research suggests that to mitigate the risk of cancer in children conceived through sperm donation, it is essential to establish family limits on the number of births per donor, enhance genetic screening processes, and consider specialized testing for rare mutations like TP53 that can escalate cancer risks.
What lessons can be learned from the case of the sperm donor carrying the TP53 mutation?
This case highlights the necessity for improved genetic screening protocols in sperm donation, as many donors could carry undetectable mutations that pose significant health risks. It calls for ongoing discussions and initiatives to refine screening practices and potentially incorporate advanced genetic testing to better safeguard future generations.
What is Li-Fraumeni syndrome, and how is it related to sperm donor genetic mutation?
Li-Fraumeni syndrome is a rare genetic disorder caused by mutations in the TP53 gene that substantially increases an individual’s risk of developing various cancers, often at a young age. Its link to sperm donor genetic mutations emphasizes the critical need for thorough screening and caution in sperm donation practices.
Why are current sperm donation screening methods insufficient for detecting rare genetic mutations?
Current sperm donation screening methods focus primarily on common genetic and infectious diseases, which may leave rare mutations like TP53 undetected. As a result, some sperm donors may unknowingly carry harmful genetic variants that could affect the health of their biological offspring.
What actions are being taken to revise sperm donation guidelines in light of genetic mutation findings?
In light of findings related to genetic mutations in sperm donors, there is a push for revising sperm donation guidelines to include international limits on donor birth numbers, improved genetic screening protocols, and increased awareness regarding the genetic risks associated with sperm donation.
| Key Point | Details |
|---|---|
| Donor’s Genetic Mutation | A rare cancer-causing mutation (TP53) linked to Li-Fraumeni syndrome was found in a European sperm donor. |
| Cancer Cases | 10 of the 67 conceived children developed various cancers, including leukemia and non-Hodgkin lymphoma. |
| Screening Limitations | Standard screening methods could not detect the TP53 mutation, raising concerns about genetic diseases in donor children. |
| Recommendations for Testing | Experts suggest genetic counseling for affected children, highlighting the need for improved donor testing methods. |
| Sperm Donation Policies | Though European sperm banks impose limits (75 families), no legal limits apply in the U.S., with ASRM recommending a maximum of 25 births per donor. |
| Health Screening Procedures | Donors undergo comprehensive screenings, including medical history and testing for infectious diseases. |
Summary
Sperm donor genetic mutation has emerged as a critical issue following reports linking a rare mutation in a European sperm donor to cancer diagnoses in multiple children conceived through his sperm. Despite rigorous health screenings, this incident emphasizes the limitations of current genetic testing methods in identifying undetectable mutations like TP53. It raises critical questions about the adequacy of donor screening regulations and the need for family limits to mitigate the risks of passing on hereditary conditions. The discussion surrounding sperm donor genetic mutation is essential to ensure safer reproductive practices for future generations.