mRNA Vaccine for Pneumonic Plague Offers 100% Effectiveness
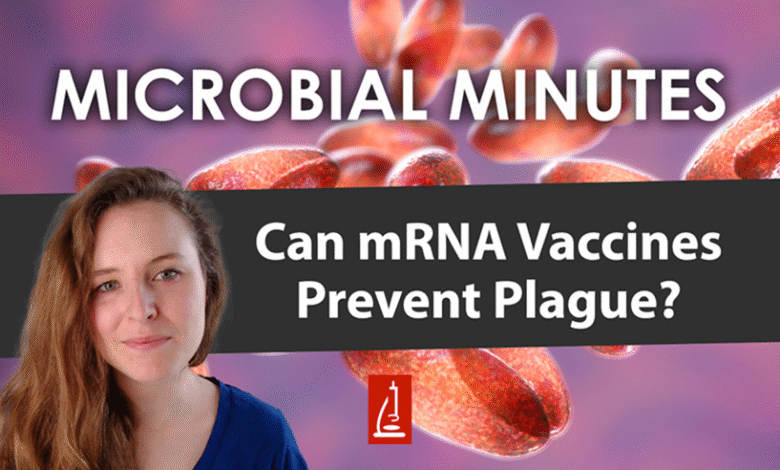
The recent breakthrough in mRNA vaccine for pneumonic plague marks a transformative leap in bacterial vaccine research, as Israeli researchers proudly announce a vaccine proving “100% effective” against Yersinia pestis, the highly lethal bacterium causing this dire lung infection. With no approved pneumonic plague vaccine currently available, this innovative development not only addresses a significant public health concern but also opens the door to a new realm in mRNA vaccine development. The research emanating from Tel Aviv University showcases the ability of mRNA technology to elicit a robust immune response against a bacterial pathogen, reshaping the way we approach infectious diseases historically deemed insurmountable. Furthermore, this advancement represents a critical step in combatting antibiotic-resistant bacteria that challenge the efficacy of traditional treatments. In an era where emerging infectious threats loom large, the implications of this mRNA vaccine could pave the way for a future where serious bacterial infections are met with powerful and effective prevention strategies.
Exploring innovative solutions to infectious diseases, the introduction of an mRNA vaccine aimed at combating pneumonic plague offers a remarkable scientific achievement. This unprecedented vaccine not only addresses the pathogenic properties of Yersinia pestis but also demonstrates the versatility and potential of mRNA technology beyond viral applications. The researchers behind the vaccine have taken significant strides in bacterial vaccine research, aiming to improve our defenses against one of the most deadly infections known to humankind. Additionally, this research highlights an important response to the challenge posed by antibiotic-resistant bacteria, suggesting a proactive approach to ensuring public health safety. The advent of such vaccines promises to enhance our preparedness against future bacterial pandemics, transforming the landscape of infectious disease control.
Understanding Pneumonic Plague and its Threat
Pneumonic plague is one of the most severe manifestations of the plague caused by the bacterium Yersinia pestis. Transmitted through respiratory droplets, this highly infectious disease can lead to rapid onset of severe lung infection, resulting in death within days if not treated promptly. Historically, outbreaks of pneumonic plague have caused significant mortality rates, prompting ongoing research for effective prevention strategies and treatments. The fear associated with potential bioterrorism applications of Yersinia pestis only amplifies the urgency of developing effective vaccines against this formidable pathogen.
Given the increasing threat of antibiotic-resistant bacteria, pneumonic plague remains a public health concern. Traditional antibiotics can be ineffective against resistant strains, making vaccination a critical component of disease prevention. Recent advancements in vaccine development, such as the mRNA technology pioneered by Israeli researchers, promise a new frontier in combating diseases like pneumonic plague, potentially offering safe and effective immunity against a bacterium known for its lethality.
Frequently Asked Questions
What is the significance of the new mRNA vaccine for pneumonic plague developed by Israeli researchers?
The new mRNA vaccine for pneumonic plague, developed by Tel Aviv University researchers, is significant as it demonstrated ‘100% protection’ against Yersinia pestis, the bacterium responsible for pneumonic plague. This breakthrough indicates a major advancement in mRNA vaccine development, which until now was primarily focused on viral pathogens.
How does the mRNA vaccine for pneumonic plague work against bacterial infections like Yersinia pestis?
The mRNA vaccine for pneumonic plague works by introducing bacterial proteins that stimulate a robust immune response. Unlike traditional vaccines that target viruses, this novel approach combines bacterial proteins with human protein segments to ensure stability and efficacy, thus training the immune system to defend against the lethal bacterium Yersinia pestis.
Are there any current approved vaccines for pneumonic plague caused by Yersinia pestis?
Currently, there are no approved vaccines specifically for pneumonic plague caused by Yersinia pestis. The mRNA vaccine developed by researchers is the first of its kind and represents a promising development in bacterial vaccine research, especially in addressing the threat of antibiotic-resistant bacteria.
What role does the lipid nanoparticle (LNP) platform play in the mRNA vaccine for pneumonic plague?
The lipid nanoparticle (LNP) platform is crucial in the mRNA vaccine for pneumonic plague as it facilitates the delivery of the mRNA into human cells. This technology, which has been effectively used in COVID-19 vaccines, allows for improved stability and a strong immune response against the Yersinia pestis bacterium.
What potential does the mRNA vaccine for pneumonic plague have in addressing future bacterial pandemics?
The mRNA vaccine for pneumonic plague has the potential to expedite the development of vaccines against 다양한 bacterial diseases. If a bacterial pandemic arises, this innovative technology could facilitate rapid vaccine production, particularly for diseases caused by pathogenic and antibiotic-resistant bacteria, thereby enhancing global pandemic preparedness.
What were the results of the animal tests conducted with the mRNA vaccine for pneumonic plague?
In animal tests, the mRNA vaccine for pneumonic plague showed remarkable results: all vaccinated animals survived and remained healthy while unvaccinated ones perished within a week of infection with Yersinia pestis. This verifies the vaccine’s efficacy and potential as a protective measure against this deadly bacterium.
How may the research on the mRNA vaccine for pneumonic plague impact future vaccine strategies?
The research on the mRNA vaccine for pneumonic plague may revolutionize future bacterial vaccine strategies by providing a new framework for developing effective vaccines against various bacterial pathogens, especially those that are antibiotic-resistant. This study highlights the flexibility and potential of mRNA technologies beyond viral applications.
What challenges still exist regarding the storage and distribution of the mRNA vaccine for pneumonic plague?
One primary challenge regarding the mRNA vaccine for pneumonic plague is the need for cold chain logistics, as it is based on the lipid nanoparticle platform recently approved for COVID-19 vaccines. Researchers are currently working on optimizing lipid formulation stability to enable room-temperature storage for broader distribution.
| Key Points |
|---|
| Israeli researchers have developed an mRNA vaccine that is 100% effective against Yersinia pestis, the bacterium causing pneumonic plague. |
| The vaccine demonstrated full protection during animal trials, where unvaccinated animals died while vaccinated ones thrived. |
| Pneumonic plague is a severe lung infection and the most dangerous form of plague. |
| Currently, no approved vaccines against Yersinia pestis exist, and it is classified as a potential bioterror weapon. |
| The study shows that mRNA vaccines can effectively trigger immune responses against bacteria, not just viruses. |
| The research may expedite the development of vaccines for other bacterial diseases, especially those resistant to antibiotics. |
| The findings were published in the journal Science Advances, highlighting the innovative approach to vaccine development. |
Summary
The development of the mRNA vaccine for pneumonic plague marks a significant advancement in medical science, showcasing the potential of mRNA technology beyond viral infections. Researchers at Tel Aviv University have demonstrated that this new vaccine offers 100% protection against the deadly bacterium Yersinia pestis, thus paving the way for future vaccines against various bacterial diseases and addressing the critical issue of antibiotic resistance. With no current approved vaccine against the plague, this breakthrough not only enhances our readiness for bioterror threats but also sets a precedent for rapid vaccine development, which is crucial in today’s pandemic-prone world.