Heart Disease Death Rates Show Dramatic Decline and Challenges
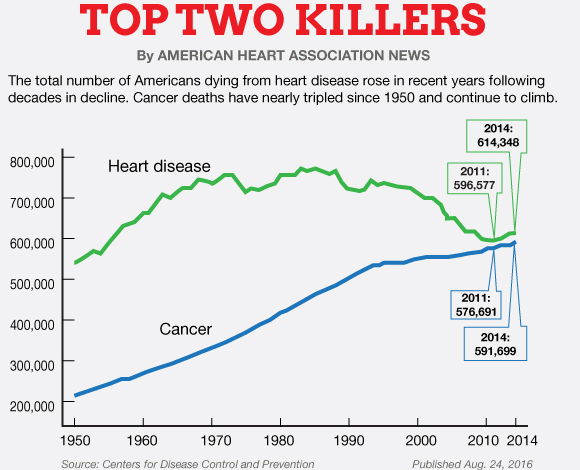
Heart disease death rates have shown notable changes over the past few decades, highlighting a significant decline in fatalities due to heart attacks. According to a recent study by the American Heart Association (AHA), overall death rates related to heart disease have decreased by an impressive 66%, with deaths from heart attacks dropping by nearly 90%. However, this positive trend is countered by an uptick in deaths from other forms of cardiovascular disease, including heart failure, arrhythmias, and hypertensive heart disease. Researchers have identified that while heart attacks accounted for over half of heart disease deaths in 1970, this percentage has fallen dramatically to only 29% by 2022. The shift underscores a critical evolving landscape in cardiovascular health, demanding increased attention to the management and prevention of these rising heart disease-related fatalities.
The rising figures surrounding fatal cardiovascular conditions signal a transformation in how we address heart health. Often referred to as the leading cause of death in modern society, fatalities stemming from heart complications such as heart failure, arrhythmias, and high blood pressure-related heart disease remain a pressing issue. Despite the remarkable advancements in reducing heart attack fatalities, the emergence of other heart-related threats requires urgent focus from the medical community. A deeper understanding of heart health, lifestyle factors, and preventive measures is crucial to combat this evolving crisis. As health experts advocate for a comprehensive approach to managing these issues, awareness regarding the broader spectrum of cardiovascular disease has never been more important.
Understanding Heart Disease Death Rates
Heart disease remains a pressing health issue, despite the notable reductions in heart attack deaths due to advances in medical treatment. The American Heart Association (AHA) reported a dramatic 66% decline in overall heart disease death rates, with heart attack-related fatalities plummeting by nearly 90%. However, this decline highlights a shifting landscape of cardiovascular health, where other forms such as heart failure and arrhythmias are now on the rise. Public awareness and understanding of these evolving statistics are crucial in shaping prevention efforts and healthcare policy.
The data reveals a significant transformation in the types of heart disease that lead to mortality. In 1970, heart attacks accounted for over half of heart disease deaths, whereas by 2022, this figure had decreased to 29%. This shift indicates the effectiveness of improved intervention strategies and highlights the need to focus on other cardiovascular diseases. As health professionals, it’s vital to educate patients on the dangers of conditions like heart failure, hypertensive heart disease, and arrhythmias, which together are now responsible for the majority of heart disease deaths.
The Rise of Other Cardiovascular Diseases
While heart attack mortality rates have beautifully declined, the rise of other cardiovascular diseases is a worrying trend. Heart failure, arrhythmias, and hypertensive heart disease contribute significantly to overall heart disease death rates, indicating a need for increased healthcare resources and prevention strategies in these areas. Specifically, heart failure—a chronic condition where the heart cannot pump sufficient blood to meet the body’s needs—has seen a substantial increase over the past several decades, correlated with the aging population and rising obesity rates.
Similarly, arrhythmias such as atrial fibrillation (AFib) present complex challenges for medical professionals. These irregular heartbeats can lead to severe complications like stroke and heart failure, yet they often go unrecognized until significant damage has been inflicted. Therefore, ongoing education and awareness campaigns are essential to ensure that patients are proactive about recognizing symptoms and seeking treatment before complications develop.
Factors Driving the Decline in Heart Attack Deaths
The decline in heart attack deaths can be attributed to several critical factors. Firstly, advancements in medical interventions, including improved emergency response protocols like bystander CPR and automated external defibrillators (AEDs), have played a crucial role. Moreover, innovations in cardiac treatments, such as coronary artery bypass grafting and better pharmaceutical options for managing heart disease, have bolstered patient outcomes significantly.
Additionally, a cultural shift towards healthier living has contributed positively to heart attack death rates. Initiatives encouraging regular physical activity, proper weight management, and smoking cessation have galvanized public health efforts to reduce cardiovascular risk. These lifestyle modifications have not only added years to lives but improved the quality of life for countless individuals at risk for heart disease.
Heart Attack Statistics Over the Years
When examining heart attack statistics over the years, the change in trends is striking and noteworthy. For example, in 1970, heart attacks were responsible for 54% of all heart disease deaths, whereas by 2022, this number decreased to just 29%. This reduction underscores the effectiveness of healthcare improvements and preventive measures, emphasizing success in treating and managing ischemic heart disease.
Such statistics shed light on the urgent need to reevaluate how we allocate resources toward cardiovascular health. As heart attacks become less fatal, the community must pivot its focus towards other forms of cardiovascular disease, including heart failure and hypertensive heart disease, ensuring we continue to save lives across the spectrum of heart-related ailments.
Emerging Challenges in Heart Disease Management
The remarkable progress in managing heart attacks has not diminished the emerging challenges posed by other cardiovascular diseases. As the data from the AHA indicate, deaths from heart failure, arrhythmias, and hypertensive heart disease are becoming increasingly prevalent. This shift suggests that while strides have been made in treating acute cardiac events, the healthcare community must adapt to address the complex needs of patients suffering from chronic heart ailments.
The evolving landscape of heart disease calls for innovative treatment strategies and comprehensive management approaches. Physicians must emphasize the importance of preventive care, regular monitoring of chronic conditions, and patient education to deal with these ongoing challenges. Coordinated care involving cardiologists, general practitioners, and dietitians can help enhance patient outcomes and introduce timely interventions to manage various cardiovascular diseases.
Lifestyle Modifications and Heart Health
Lifestyle modifications remain an integral component of maintaining cardiovascular health. The AHA’s ‘Life’s Essential 8’ provides a framework for individuals to evaluate their health behaviors, encouraging improvements in diet, activity level, and overall wellness. Individuals who adopt healthier lifestyles may see significant reductions in their risk of developing heart disease, especially heart failure and hypertensive heart disease, which currently represent a growing segment of heart disease fatalities.
Encouraging long-term changes such as regular exercise, healthy eating habits, and effective stress management can mitigate the effects of poor lifestyle choices. Additionally, addressing obesity and related conditions like type 2 diabetes through community initiatives and educational programs can lead to a healthier population and potentially reduce heart disease death rates in future generations.
The Evolving Role of Healthcare Providers
Healthcare providers play a crucial role in addressing the current landscape of heart disease and must remain vigilant in guiding patients toward optimal heart health. With heart attacks becoming less common as a cause of mortality, the focus of medical professionals must shift to tackling other cardiovascular conditions. Comprehensive patient assessments and tailored treatment plans are essential to manage chronic diseases such as heart failure and arrhythmias.
Moreover, healthcare providers must foster collaborative relationships with patients to promote better adherence to treatment plans. By enhancing communication and understanding of patient needs, doctors can empower individuals to take charge of their health, leading to improved outcomes and potentially reducing the heart disease death rates associated with non-ischemic conditions.
Future Directions in Cardiovascular Research
As we confront the challenges surrounding cardiovascular diseases, ongoing research will be vital in developing innovative treatment modalities and prevention strategies. The emergence of technologies and methodologies in cardiology—such as telemedicine, cardiac rehabilitation programs, and novel pharmaceuticals—offers new hope for improving heart health outcomes. Future research should prioritize a holistic understanding of the factors contributing to heart diseases, including genetics, lifestyle, and socio-economic status.
Investigating demographic differences and the unique needs of diverse populations can also inform targeted interventions and resource allocations. As cardiovascular disease remains a leading cause of death in the U.S., understanding its evolving nature and the factors influencing patient outcomes will ultimately pave the way for improved clinical practices and patient-centered care.
Frequently Asked Questions
What are the current heart disease death rates in the U.S.?
As of 2022, heart disease remains the leading cause of death in the U.S., accounting for over 900,000 fatalities. Although heart attack death rates have plummeted by nearly 90% over the last 50 years, other cardiovascular diseases such as heart failure, hypertensive heart disease, and arrhythmias now account for 47% of heart disease deaths.
How have heart attack statistics changed over the past 50 years?
Heart attack statistics show a remarkable decline, with deaths from heart attacks—previously over 54% of heart disease deaths in 1970—dropping to only 29% in 2022. This significant reduction in heart attack deaths reflects advancements in treatment and preventive measures.
What is the impact of hypertension on heart disease death rates?
Hypertensive heart disease, caused by long-term high blood pressure, has significantly contributed to rising death rates due to cardiovascular disease. In 2022, this condition, alongside heart failure and arrhythmias, was responsible for 47% of heart disease-related deaths, indicating a shift in the causes of heart disease mortality.
What role do arrhythmias play in heart disease death rates?
Arrhythmias, or irregular heartbeats, have become more prevalent as a cause of death, accounting for an increasing percentage of heart disease fatalities. As medical management improves for heart attacks, attention is shifting to manage conditions like atrial fibrillation, which significantly contributes to overall heart disease death rates.
What are the factors contributing to the increase in heart failure deaths?
The rise in heart failure deaths is attributed to several factors, including an aging population and increased incidence of chronic conditions like obesity and type 2 diabetes. These factors complicate overall cardiovascular health, contributing to a larger share of heart disease death rates.
How has lifestyle change influenced heart disease death rates?
Lifestyle changes such as quitting smoking, regular exercise, and managing diet have greatly influenced heart disease death rates, particularly in reducing heart attack risk. However, ongoing issues like obesity and physical inactivity pose significant challenges to maintaining these improvements in heart-related mortality.
What are ‘Life’s Essential 8’ and how do they relate to heart disease prevention?
‘Life’s Essential 8’ is a set of cardiovascular health metrics defined by the American Heart Association related to lifestyle choices, including diet, physical activity, weight management, and smoking cessation. Improving these metrics is crucial in preventing heart disease and reducing overall heart disease death rates.
Why is heart disease death rate data important for public health?
Heart disease death rate data is vital for public health as it highlights trends, identifies at-risk populations, and informs interventions. With heart disease being the leading cause of death, understanding mortality patterns aids in effective resource allocation and prevention strategies.
| Key Points | Details |
|---|---|
| Heart Disease Death Rates | Overall heart disease-related death rates have declined by 66% over recent years. |
| Heart Attack Deaths | Heart attack deaths have dropped by almost 90%. In 1970, they accounted for 54% of heart disease deaths. |
| Emerging Types of Heart Disease | Heart failure, arrhythmias, and hypertensive heart disease have seen increased mortality rates, responsible for 47% of heart disease deaths in 2022. |
| Lifestyle Factors | Improvements in lifestyle, treatment advancements, and preventive measures contribute to the decline in heart attack deaths. |
| Challenges Ahead | Despite the decline in heart attack mortality, challenges remain with managing other forms of cardiovascular disease. |
Summary
Heart disease death rates have seen significant changes, with a marked decline in heart attack fatalities. While advancements in medical treatment and healthier lifestyles have led to a 66% decrease in overall heart disease death rates, the rise in fatalities from other cardiovascular diseases, such as heart failure and arrhythmias, presents new challenges. Continued attention is needed to manage these emerging threats to heart health, emphasizing the importance of prevention and treatment strategies.