Gabapentin and Dementia: New Study Reveals Alarming Risks
Recent research has linked gabapentin and dementia, raising important questions about the safety of this commonly prescribed medication. Gabapentin, widely used for managing chronic pain—especially neuropathic pain—may inadvertently increase the risk of neurodegeneration in certain patients. Studies published in the journal Regional Anesthesia & Pain Medicine indicate that individuals taking gabapentin are more than twice as likely to develop dementia or mild cognitive impairment within ten years, a concerning trend that calls for further investigation. The side effects associated with gabapentin could be more severe than previously understood, warranting caution among healthcare providers when prescribing chronic pain medications. Alongside exercise and dementia prevention strategies, understanding the implications of cognitive impairment studies on gabapentin usage is crucial for safeguarding neurological health.
In exploring the relationship between gabapentin and cognitive decline, it is essential to consider alternative descriptors such as the effects of chronic pain relievers on neurocognitive health. Multiple studies have uncovered potential connections between these medications and an increased risk of memory disorders, emphasizing the importance of vigilance when prescribing such treatments. Patients who have utilized gabapentin for managing uncomfortable conditions like neuropathic pain may face unforeseen consequences regarding their mental acuity over time. With growing evidence associating certain pain medications with the onset of dementia and mild cognitive impairment, tailored approaches to pain management that prioritize both physical and cognitive well-being are imperative. Focusing on preventative measures like physical exercise can play a vital role in mitigating these risks and enhancing overall cognitive function.
The Link Between Gabapentin and Cognitive Impairment
Recent studies have highlighted a concerning association between gabapentin use and cognitive impairment, particularly regarding neurodegenerative diseases like dementia. Gabapentin, initially praised for its effectiveness in managing chronic pain, especially in cases of neuropathic pain, has drawn scrutiny as newer research uncovers data linking its long-term use with significant cognitive risks. The recent study published in the journal Regional Anesthesia & Pain Medicine indicates that adults prescribed gabapentin are at a higher risk for developing mild cognitive impairment and dementia within a decade of usage.
The implications of these findings are profound, especially for younger adults aged 18 to 64 who might not typically be considered at risk for such conditions. While gabapentin is often viewed as a safer alternative to opioids, the potential side effects warrant careful consideration. This raises an essential question: Should the prescription of healthcare providers adapt in light of these findings? More extensive cognitive impairment studies are needed to establish clearer guidelines around the use of gabapentin in pain management.
Chronic Pain Medications and Their Side Effects
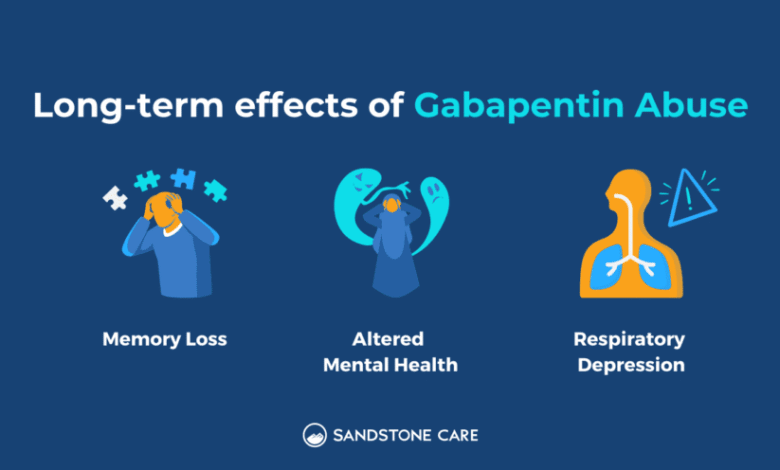
Chronic pain medications, including gabapentin, often come with a range of side effects that can significantly impact patients’ quality of life. While many turn to gabapentin for relief from persistent pain, they may not be fully aware of the long-term consequences that can arise. These side effects extend beyond mere discomfort, venturing into cognitive challenges that could hinder patients’ daily operations and overall mental well-being. It’s crucial for patients to be informed about these risks before initiating treatment with chronic pain medications.
Furthermore, medical professionals must prioritize thorough discussions concerning the potential trade-offs associated with using gabapentin over time. As the risks of neurodegeneration and cognitive decline become more evident, practitioners may need to consider alternative therapies or complementary strategies, such as exercise and lifestyle modifications. The latter has shown promise in reducing dementia risk, emphasizing the need for a holistic approach to chronic pain management.
Preventing Dementia Through Lifestyle Changes
Research consistently supports the notion that lifestyle choices play a pivotal role in preventing dementia. Exercise, in particular, has garnered attention for its role in lowering the risk of neurodegenerative diseases. Engaging in regular physical activity can enhance cognitive function, promote brain health, and potentially offset some of the adverse effects associated with chronic pain medications like gabapentin. Incorporating regular exercise into one’s routine could serve not only as a pain management tool but also as a preventative measure against cognitive decline.
Incorporating physical activity does not imply an all-or-nothing approach; even moderate levels of exercise can yield significant benefits. The impact of exercise on the brain is profound, stimulating neuroplasticity and promoting healthier brain aging. As findings continue to emerge linking cognitive health to a proactive lifestyle, those utilizing medications for chronic pain should consult healthcare professionals for integrative strategies that include physical activity.
Gabapentin Use in Younger Populations
The growing trend of gabapentin prescriptions in younger populations has raised alarms within the medical community. While the medication has become a go-to solution for managing lower back pain, younger adults, who were previously not seen as vulnerable to cognitive decline, are now being documented in studies indicating an increased risk of developing dementia-related conditions. As evidenced by the research, this demographic, aged predominantly between 18 and 64, could unknowingly face severe consequences stemming from this commonly prescribed medication.
With more than double the likelihood of developing mild cognitive impairment or dementia within ten years of gabapentin usage, there is a critical need for heightened awareness and communication regarding the long-term implications of this medication. Proper assessment of younger patients’ prescriptions becomes essential to ensure they are not prescribed treatments that may inadvertently jeopardize their cognitive health.
The Importance of Monitoring Gabapentin Prescriptions
The findings from recent studies underscore the necessity of monitoring patients who are prescribed gabapentin, especially for chronic pain conditions. Given the observed correlation between the frequency of prescriptions and the likelihood of developing cognitive issues, healthcare providers must engage in proactive evaluation and follow-ups. Knowing that those who receive multiple prescriptions face heightened risks, it is imperative that clinicians assess the cumulative effects of gabapentin over time.
Close monitoring can involve regular cognitive assessments and discussions about any perceived changes in mental clarity. By fostering an open dialogue, patients can feel empowered to report any concerns, thus fostering a collaborative approach to pain management. Ultimately, addressing the potential cognitive decline associated with gabapentin may lead to more balanced management of chronic pain, reducing the likelihood of dementia and improving overall patient outcomes.
Gabapentin vs. Other Chronic Pain Options
As concerns about gabapentin’s side effects loom large, it is important to explore other chronic pain management options. Traditional pain management therapies, including opioid prescriptions, might bear their own sets of risks, yet they do not appear to carry the same weight of neurodegenerative concerns as gabapentin. Patients deserve comprehensive assessments of the benefits and drawbacks of each potential medication, leading to the most informed decision possible.
Non-pharmacological therapies, such as physical therapy and acupuncture, also provide valuable alternatives without the cognitive risks associated with gabapentin. Furthermore, integrating therapeutic approaches, including cognitive behavioral therapy or mindfulness practices, may enhance patient wellness while addressing pain effectively. By diversifying treatment plans, healthcare providers can mitigate the developmental risks while maximizing patient relief.
The Role of Research in Understanding Gabapentin Side Effects
Continued research into the side effects of gabapentin is essential for developing a clearer understanding of its impacts on cognitive health. The retrospective nature of recent studies highlights the need for ongoing examination and additional trials to solidify evidence regarding the connections between gabapentin, its side effects, and the risk of neurodegeneration. This insight will not only help inform healthcare practices but also empower patients in their health journeys.
Research findings must be utilized to foster patient education, ensuring individuals make informed choices about their chronic pain management strategies. While gabapentin may offer relief in the short term, the long-term implications merit careful consideration. Building a foundation of understanding through research will guide both clinicians and patients towards better health management practices.
Understanding Cognitive Impairment Studies
Cognitive impairment studies play a critical role in illuminating the connections between lifestyle factors and brain health, particularly among those utilizing medications such as gabapentin. By examining diverse patient populations and their prescribed treatments, researchers can provide valuable insights into how various chronic pain medications affect cognitive functions over time. These studies can help draw broader conclusions that apply to trends in medication prescribing and patient experiences.
By dissecting the nuances within cognitive impairment studies, researchers can develop strategic guidelines for healthcare providers and patients alike. These insights are crucial to forming preventative measures against cognitive decline, allowing informed adjustments to treatment plans that prioritize both pain relief and cognitive health. Fostering a proactive approach may contribute to reducing the prevalence of dementia associated with medication use.
Gabapentin Prescription Patterns: What Patients Should Know
Understanding gabapentin prescription patterns is essential for patients and healthcare providers alike. The significant rise in gabapentin prescriptions over the past few decades indicates its popularity as a treatment for chronic pain management. However, patients should be made aware of the potential links between continued use of gabapentin and risks for developing cognitive impairments, particularly as research suggests a correlation with future neurological conditions.
Awareness is the first step towards ensuring patient safety and health optimization. Patients should feel encouraged to ask their doctors questions regarding their prescriptions, especially concerning the risks associated with long-term use. By being informed about gabapentin and its implications, patients can engage in meaningful discussions with their healthcare providers and make educated decisions regarding their pain management.
Frequently Asked Questions
What is the link between gabapentin and dementia according to recent studies?
Recent studies indicate a concerning association between gabapentin prescription and an increased risk of dementia and mild cognitive impairment (MCI). Specifically, individuals aged 18 to 64 who were prescribed gabapentin for chronic pain were over twice as likely to develop dementia or cognitive impairment within 10 years compared to those not on the medication.
How does gabapentin affect cognitive function in patients treated for chronic pain?
Gabapentin, a medication often prescribed for chronic pain, has recently drawn attention for potentially impacting cognitive function. Studies have found that patients who received higher quantities of gabapentin prescriptions experienced a heightened risk of developing cognitive impairment, with a significant percentage more likely to be diagnosed with dementia after extended use.
Are there specific side effects of gabapentin that could lead to neurodegeneration?
While gabapentin is generally considered to have a low potential for addiction, emerging research has linked its long-term use to possible side effects that may contribute to neurodegeneration. The implications include increased risks for dementia and mild cognitive impairment, especially amongst patients frequently using this medication for chronic pain.
How can exercise relate to the prevention of dementia in the context of gabapentin use?
In considering gabapentin and dementia, studies suggest that regular exercise may mitigate the risk of cognitive decline. Engaging in physical activity can promote brain health and potentially counteract some of the negative cognitive effects linked to prolonged gabapentin usage, emphasizing the importance of lifestyle choices in managing dementia risk.
What precautions should be taken for patients prescribed gabapentin regarding cognitive health?
Patients prescribed gabapentin should be monitored closely for signs of cognitive decline, especially if they have received multiple prescriptions. Understanding the potential link between gabapentin and dementia can help healthcare providers and patients make informed decisions regarding pain management and cognitive health.
What other factors were considered in studies examining gabapentin and cognitive impairment?
The studies examining gabapentin’s potential link to cognitive impairment considered various factors, including demographic data, pre-existing health conditions, and the use of other chronic pain medications. This comprehensive approach helps isolate the impact of gabapentin on dementia risk.
Is the risk of dementia from gabapentin more significant in certain age groups?
Research indicates that younger adults, specifically those aged 18 to 64, may face a greater risk of developing dementia when prescribed gabapentin for chronic pain. This observation highlights the need for caution when prescribing gabapentin to younger populations.
| Key Points |
|---|
| A new study indicates that exercise can help reduce the risk of dementia. |
| Gabapentin, commonly used for pain relief, is potentially associated with a heightened risk of dementia and mild cognitive impairment (MCI). |
| Patients aged 18 to 64 prescribed gabapentin are over twice as likely to develop dementia and MCI. |
| Those with six or more prescriptions of gabapentin show a 29% higher risk of dementia and 85% higher risk of MCI within 10 years. |
| Frequency of prescriptions increases risk: patients with 12+ prescriptions show 40% higher dementia risk and 65% higher MCI risk. |
| Study had limitations, including retrospective design and inability to measure dosage or duration effects. |
| Monitoring of patients on gabapentin for cognitive decline is recommended based on the findings. |
Summary
Gabapentin and dementia are increasingly becoming topics of concern in the medical community. Recent research has established a potential link between the use of gabapentin, a medication often prescribed for chronic pain, and an increased risk of developing cognitive impairments such as dementia and mild cognitive impairment (MCI). With evidence showing that younger adults prescribed gabapentin face significantly higher risks, it is essential for healthcare providers to monitor patients closely for any signs of cognitive decline as part of their ongoing treatment.