DO vs MD: Understanding the Key Differences in Medicine
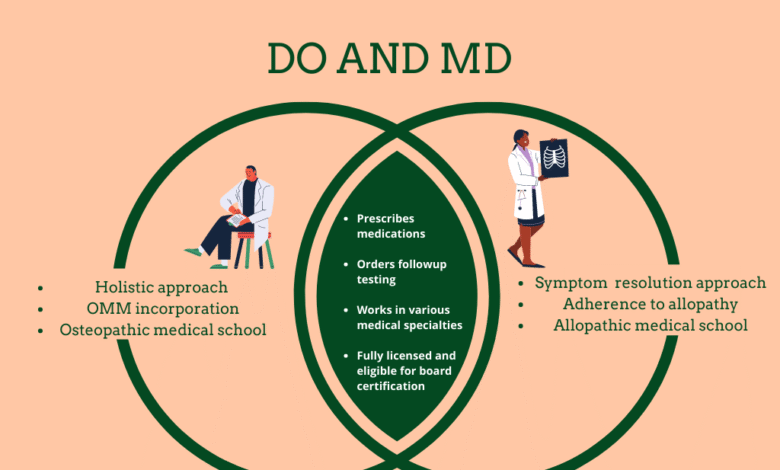
The ongoing discussion about Joe Biden’s mental ability has brought to light the distinct roles of healthcare professionals, particularly the difference between DO and MD. While both Doctors of Osteopathic Medicine (DOs) and Doctors of Medicine (MDs) undergo rigorous training and can provide comprehensive patient care, they do differ in their philosophies and approaches to treatment. DOs emphasize a holistic perspective, focusing on the interrelationships of the body’s systems, which contrasts with the more traditional, disease-centric approach of MD training. Understanding the importance of DOs in the healthcare system is vital, especially as they incorporate unique methods such as osteopathic manipulative medicine to enhance wellness. As we explore these differences in detail, the significance of both types of medical professionals in contemporary medicine remains paramount.
In the realm of healthcare, the distinction between Doctor of Osteopathic Medicine and traditional medical doctors often goes unnoticed by the general public. These two types of physicians, while sharing a foundational medical education, operate from varying perspectives, with osteopathic medicine prioritizing holistic treatment and wellness. As interest in comprehensive health approaches grows, the role of DOs becomes increasingly significant in primary care and specialized fields. The evolving landscape of medical training has led to a deeper understanding of how the methods employed by DOs can complement those of MDs, ultimately benefiting patients. This discussion brings to the forefront how both DOs and MDs contribute uniquely to patient care in today’s healthcare environment.
Understanding the Difference Between DO and MD
The distinction between a Doctor of Osteopathic Medicine (DO) and a Doctor of Medicine (MD) primarily lies in their training philosophy and approaches to patient care. Both types of physicians undergo rigorous medical education, but DOs receive additional training focusing on the holistic connection between the body, mind, and spirit. While MDs typically emphasize treating specific diseases and symptoms, DOs often consider the broader context of a patient’s life and health, adopting a more preventive approach to medicine. This difference emphasizes the unique training and approaches within the medical field.
In practice, both DOs and MDs are fully qualified physicians capable of diagnosing illnesses, prescribing medications, and performing surgeries. They both complete residency programs in specialty areas post-medical school. However, the added component of osteopathic training allows DOs to practice manipulative medicine, a hands-on treatment technique. Despite these differences, many patients may not notice a significant difference when receiving care from a DO versus an MD, reinforcing the idea that both paths lead to competent and compassionate medical professionals.
The Importance of DOs in Current Healthcare
As the healthcare landscape continues evolving, the role of Doctors of Osteopathic Medicine (DOs) has become increasingly important. With a growing emphasis on preventive care and holistic health, DOs are particularly well-suited to meet the needs of patients seeking comprehensive treatment options. They not only diagnose and treat ailments but also focus on education and preventive measures to enhance overall wellness. The unique training DOs undergo prepares them to approach patient care from multiple angles, which is becoming more critical in today’s complex healthcare environment.
Statistics indicate a rising number of DOs in the United States, with newer generations of physicians embracing this holistic approach to medicine. As of 2023, approximately 57% of DOs practice in primary care fields such as family medicine and pediatrics. This trend highlights the importance of DOs in addressing the healthcare needs of communities across the nation. Their emphasis on a patient-centered approach often leads to improved health outcomes and satisfaction among patients, demonstrating the essential role that DOs play in modern medicine.
Training and Education: DO vs MD
The training paths for DOs and MDs are quite similar but remain distinct in certain aspects. Both require a bachelor’s degree prior to enrolling in medical school, followed by four years of medical education. MDs typically follow a more traditional approach with rigorous training focused on pharmacology, surgery, and disease-centric care. Conversely, DOs delve deeper into osteopathic principles, which include an additional 200 hours of training in osteopathic manipulative treatment (OMT). This hands-on methodology enriches their clinical practice, allowing them to offer more personalized care.
After medical school, both DOs and MDs must complete residency training, which can last from three to seven years depending on the specialty. The comprehensive nature of this residency training ensures that both types of physicians are equipped to treat patients effectively. Despite their varied training philosophies, both DOs and MDs are equally respected in the medical community and can serve as primary care providers or specialists, providing essential services across diverse healthcare settings.
The Holistic Approach of Osteopathic Medicine
Osteopathic medicine is characterized by its holistic approach that considers the interconnectedness of bodily systems. DOs are trained to view patients as whole individuals rather than focusing exclusively on symptoms. This method aligns with the increased demand for personalized medical care that addresses both physical and emotional well-being. The Cleveland Clinic emphasizes that DOs aim to promote health and wellness through education and preventative strategies, incorporating lifestyle changes and alternative therapies alongside conventional treatments.
This holistic perspective of osteopathic medicine allows DOs to employ techniques such as OMT, enhancing their ability to diagnose and treat complex conditions. Patients often experience greater satisfaction, as they feel genuinely understood and cared for. As healthcare systems increasingly recognize the value of holistic treatment approaches, the demand for DOs continues to rise, particularly in fields like family medicine where comprehensive care is crucial.
The Growing Acceptance of DOs in Medicine
Historically, DOs have faced challenges and misconceptions within the medical community, but recent years have seen a growing acceptance of Osteopathic Medicine. As the healthcare landscape shifts to prioritize preventive care, the expertise of DOs is gaining recognition, with many patients and healthcare providers understanding the value of their holistic approach. The rise in patient advocacy for comprehensive care aligns seamlessly with osteopathic principles, making DOs key contributors to modern medicine.
Research from the American Osteopathic Association indicates a rising trend in the number of DOs practicing across various specialties, reflecting their growing visibility and importance in healthcare. As of 2023, approximately 70% of practicing DOs are under the age of 45, indicating a younger generation entering the field and advocating for holistic health practices that accommodate the evolving needs of patients. This trend showcases the positive evolution of DOs within the medical landscape, paving the way for a more integrative approach to health care.
DOs’ Role in Family Medicine
Family medicine is a primary area of practice for many Doctors of Osteopathic Medicine (DOs), representing nearly 57% of the field according to recent data. This specialty is particularly suited for the holistic training that DOs receive, as it allows for the application of their comprehensive approach to patient care. Family medicine practitioners are often the first point of contact for patients, making it essential for them to possess strong skills in diagnosing a wide range of conditions while also addressing preventive health practices.
Moreover, the emphasis that DOs place on lifestyle and wellness makes them ideal for managing chronic conditions prevalent in family medicine. They understand the significance of social determinants of health and work collaboratively with patients to develop long-term strategies for maintaining health and preventing illness. As more families seek holistic and preventive care options, the role of DOs in family medicine will likely continue to expand, benefiting the overall health of communities.
Advancements in Osteopathic Manipulative Medicine
Osteopathic manipulative medicine (OMM) is a vital part of a DO’s training, providing an additional layer of treatment options for managing patient care. OMM encompasses various techniques designed to alleviate pain, enhance mobility, and encourage holistic healing. By utilizing their hands, DOs can target problem areas in the body, offering treatments that can complement or even substitute for traditional medications. This method is especially beneficial for patients dealing with musculoskeletal pain and can enhance recovery outcomes.
Research continues to affirm the efficacy of OMM in various medical contexts. Studies have shown that integration of OMM can result in significant improvements in pain relief and functional outcomes for patients. As the medical community increasingly supports integrative approaches to treatment, the appreciation for OMM within both osteopathic and allopathic frameworks is likely to rise. This creates an opportunity for DOs to further promote their unique skill sets and enhance patient care methodologies.
The Historical Context of Osteopathic Medicine
Understanding the origins of osteopathic medicine reveals its foundational commitment to treating the whole person. Established in 1892 by Dr. Andrew Taylor Still, the creation of DO training was a response to the limitations he identified in conventional medicine after personal tragedies caused by illness. Still’s philosophy centered around a holistic view of health, emphasizing the interrelatedness of the body’s systems and promoting wellness through preventive care and education, which remains at the core of osteopathic training today.
The historical context of DO training also reflects its evolution, with increasing numbers of medical schools adopting osteopathic principles into their curriculums. Today’s DOs benefit from a robust integration of scientific knowledge with osteopathic philosophy, thereby addressing a broad spectrum of health needs. As patients increasingly seek comprehensive care, the historical roots of osteopathic medicine emphasize its ongoing relevance and adaptability in a changing healthcare landscape.
The Future of DOs in American Healthcare
The future of Doctors of Osteopathic Medicine (DOs) in American healthcare appears promising as the sector shifts toward more integrative and patient-centered approaches. The growing recognition of the importance of holistic care positions DOs favorably within various medical specialties, particularly with increasing patient demand for practitioners who prioritize overall well-being. As awareness of the benefits of osteopathic philosophies continues to expand, the role of DOs is likely to become increasingly vital in meeting the healthcare needs of diverse populations.
Moreover, as healthcare becomes more collaborative, the integration of DOs alongside MDs in practices will foster a richer exchange of medical philosophies, benefiting patients, and enhancing care coordination. With advancements in telemedicine and patient engagement technologies, DOs are well-positioned to leverage their unique skills to provide comprehensive care that transcends traditional healthcare boundaries. This evolution suggests a future where DOs will play a pivotal role in leading the charge towards a more holistic and integrated healthcare system.
Frequently Asked Questions
What is the difference between DO and MD in medical training?
The difference between DO (Doctor of Osteopathic Medicine) and MD (Doctor of Medicine) in medical training lies primarily in their philosophy and approach to treatment. While both DOs and MDs complete similar medical education and residency requirements, DOs emphasize a holistic approach to medicine, including a focus on the mind, body, and spirit connection. Additionally, DOs receive training in osteopathic manipulative medicine (OMM), which allows them to perform hands-on treatment techniques.
Are DOs trained to recognize mental decline like MDs?
Yes, DOs are trained to recognize mental decline just like MDs. As highlighted by Dr. Marc Siegel, a family practitioner with a DO background can screen for cognitive issues effectively. The capabilities of both DOs and MDs are essentially the same when it comes to diagnosing and addressing health concerns, including mental health.
What is the importance of DOs in the healthcare system?
The importance of DOs in the healthcare system is significant, as they provide comprehensive care that integrates traditional medical treatments with osteopathic methods. DOs often lead in primary care fields, such as family medicine and pediatrics, and contribute to a growing trend towards holistic healthcare practices that prioritize overall wellness and preventive care.
Can both DOs and MDs prescribe medication?
Yes, both DOs and MDs can prescribe medication and practice medicine in the United States. There are no restrictions on prescribing medications, allowing both types of physicians to provide comprehensive medical care to their patients regardless of their degree.
Do MDs have a different approach to patient care compared to DOs?
Yes, MDs typically have a more traditional approach centered on a biomedical model, focusing primarily on diagnosing and treating diseases with medications and surgeries. In contrast, DOs tend to take a more holistic approach, emphasizing the treatment of the whole person and incorporating preventive care and education into their practice.
What unique training do DOs receive compared to MDs?
DOs undergo unique training in osteopathic manipulative treatment (OMT), which involves hands-on techniques to diagnose and treat various conditions. This additional training focuses on the musculoskeletal system and encourages DOs to consider a more holistic view of patient care, integrating physical manipulation with conventional medical practices.
How many osteopathic medical schools are there compared to allopathic medical schools?
As of 2023, there are 38 osteopathic medical schools (granting DO degrees) and 154 allopathic medical schools (granting MD degrees) in the U.S. The growth in the number of osteopathic schools reflects an increasing recognition of the importance of DOs in modern medicine.
What specialties do most DOs practice compared to MDs?
Most DOs tend to practice in primary care fields, with about 57% working in family medicine, internal medicine, and pediatrics. In contrast, only 28% of MDs work in these specialties, highlighting the growing role of DOs in primary healthcare delivery.
| Key Points | DO (Doctor of Osteopathic Medicine) | MD (Doctor of Medicine) |
|---|---|---|
| Personal physician of Joe Biden, Kevin O’Connor, testified regarding mental capability. | Focuses on holistic treatment and includes osteopathic manipulative methods. | Utilizes all types of modern medical treatments, primarily allopathic medicine. |
| Training emphasizes mind-body-spirit connection. | DOs undergo additional training in OMM (Osteopathic Manipulative Medicine). | More focused on conventional medical practices and interventions. |
| 675 DOs remain actively practicing and have been increasingly prevalent in recent years. | Established schools focused on holistic and preventive care. | More traditional medical schools focused on drug and surgery treatments. |
| DOs represent about 57% of practitioners in family medicine, internal medicine, and pediatrics. | Training originated in 1892 and aims to treat patients comprehensively. | MDs constitute about 28% of the same practice areas. |
Summary
DO vs MD are both essential medical disciplines in the healthcare system, with each offering distinct philosophies and training methodologies. A Doctor of Osteopathic Medicine (DO) emphasizes a holistic approach, focusing on the interconnection between the mind, body, and spirit while incorporating hands-on techniques like osteopathic manipulative treatment. Conversely, a Doctor of Medicine (MD) primarily engages with allopathic methods, treating ailments predominantly through medication and surgery. Both DOs and MDs have similar educational backgrounds and can provide comprehensive medical care, but their training and approaches can differ significantly, catering to diverse patient needs.