Prevent Belly Fat: Understand Causes and Solutions

Preventing belly fat is an essential goal for many, especially as we age and face the challenges associated with weight gain. Research shows that aging stem cells can boost fat cell production, leading to an increase in belly fat, a common issue for older adults. However, understanding the causes of belly fat, including stress and poor sleep, can help inform effective strategies for healthy aging. Incorporating lifestyle changes such as a protein-rich diet and stress management can significantly reduce belly fat while promoting overall wellness. By taking proactive steps, individuals can combat the inevitability of weight gain with age and maintain a more fit physique.
Addressing abdominal weight gain is crucial for those navigating the complexities of aging. As we grow older, the body undergoes various changes that can lead to unhealthy levels of visceral fat, especially around the waist. Factors like heightened stress levels and insufficient sleep contribute to the challenges of managing body weight in later years. By adopting healthy habits and making informed dietary choices, individuals can effectively manage fat cell production and improve their overall health outcomes. Emphasizing balanced nutrition and wellness practices is key to thwarting the expansion of waistlines and ensuring a healthier aging trajectory.
Understanding Belly Fat Causes as We Age
As we age, the causes of belly fat become more complex and multifaceted. Research shows that aging stem cells, particularly adipocyte progenitor cells (APCs), play a significant role in the production of fat cells, especially in the abdominal region. Older adults often experience an increase in these cells’ activity, leading to excess fat storage. This phenomenon is complemented by hormonal changes and a decrease in metabolic rate, making it easier to accumulate belly fat as we grow older.
Additionally, lifestyle factors such as increased stress and poor sleep further exacerbate these conditions. High cortisol levels, for instance, are linked with increased fat storage in the abdominal area. As a result, understanding these underlying causes is crucial for developing effective strategies to combat unwanted belly fat and promote healthy aging.
The Connection Between Weight Gain and Age
It’s a common observation that many individuals notice weight gain as they age, especially around the waist. This change is not merely a result of a sedentary lifestyle but is intricately linked to biological processes within the body. Aging is associated with a natural decline in muscle mass, which slows the metabolism and alters fat distribution. As muscle mass decreases, the body requires fewer calories, leading to weight gain if dietary habits remain unchanged.
Moreover, the accumulation of visceral fat, which is fat stored in the abdomen, poses additional health risks. It is known to be more metabolically active than subcutaneous fat, increasing the risk of several age-related diseases. As such, understanding and addressing the factors that contribute to age-related weight gain is essential for maintaining overall health and preventing belly fat.
Strategies to Prevent Belly Fat
Preventing belly fat, particularly as we age, involves a proactive approach to health and nutrition. One of the most effective strategies is to prioritize protein intake. Consuming adequate protein helps maintain lean muscle mass, which is essential for a healthy metabolism. Experts suggest starting the day with a hearty dose of protein, which can help keep you satisfied longer, stabilize blood sugar levels, and reduce the likelihood of unwanted fat accumulation.
In addition to protein, managing stress and optimizing sleep are critical components of reducing belly fat. Chronic stress can lead to hormonal imbalances that encourage fat storage. Thus, implementing relaxation techniques, such as mindfulness and regular physical activity, can greatly contribute to better weight management. By prioritizing these strategies, individuals can effectively combat belly fat and promote healthier aging.
The Role of Healthy Aging in Fat Control
Healthy aging involves not just the absence of illness but also the presence of well-being and functional ability. As we age, maintaining health is crucial in controlling belly fat and preventing metabolic disorders. Engaging in regular physical activity helps to preserve muscle mass and improve metabolic health, thereby reducing the risk of fat accumulation around the abdomen.
Furthermore, adopting a balanced diet rich in whole foods and minimizing processed options can dramatically influence fat cell production and overall health. The body’s aging process can be mitigated by lifestyle choices that support both physical and mental health, allowing for more effective control over belly fat and supporting a more vibrant, active life.
Minimizing Processed Carbs to Reduce Belly Fat
One of the surprising factors contributing to belly fat accumulation is the consumption of ultraprocessed carbohydrates and refined sugars. These foods not only contribute to increased insulin resistance but also promote inflammatory responses in aging adipose tissue. By minimizing these types of foods in your diet, you can effectively reduce belly fat accumulation and improve your overall metabolic health.
Swapping out refined carbohydrates for whole grains, fruits, and vegetables can have a significant impact on weight management. This dietary adjustment not only aids in controlling body fat but also fuels the body with essential nutrients necessary for healthy aging. Incorporating an array of whole foods can help to stabilize blood sugar and minimize the risk of weight gain as we navigate the aging process.
The Science Behind Fat Cell Production
Recent research has provided pivotal insights into why aging is associated with increased fat cell production. Studies have shown that the adipocyte progenitor cells (APCs) become more active as one ages, resulting in a higher number of fat cells being produced. This biological shift underlies the significance of managing your diet and lifestyle choices to prevent excess belly fat accumulation.
Understanding this process can inform strategies for fat management. For instance, targeting inflammation and hormonal balance can help in regulating APC activity. This approach underscores the importance of taking a comprehensive view of health, focusing on nutrition, exercise, and emotional well-being to combat age-related belly fat production.
Managing Stress for Better Health Outcomes
Chronic stress plays a significant role in weight gain and belly fat accumulation. Elevated cortisol levels, associated with stress, can lead to increased appetite and cravings for unhealthy foods, exacerbating the challenge of maintaining a healthy waistline as we age. Moreover, stress can disrupt sleep patterns, further complicating weight management.
Implementing stress reduction techniques such as yoga, meditation, or even simple breathing exercises can help regulate cortisol levels, potentially leading to healthier fat distribution. Reducing stress not only aids in managing belly fat but also contributes to overall well-being, making it a critical component of a health-focused lifestyle.
Prioritizing Sleep for Weight Management
Quality sleep is often overlooked yet remains a foundational element in preventing belly fat, especially as we age. Research indicates that inadequate sleep can lead to hormonal imbalances, increased hunger hormones, and decreased satiety, resulting in greater calorie consumption and fat storage around the abdomen. Experts recommend striving for seven to nine hours of restorative sleep per night.
Establishing a regular sleep routine and creating a restful environment can greatly enhance sleep quality. This, in tandem with proper nutrition and exercise, becomes a crucial strategy in combating belly fat and promoting healthier aging. A mindful approach to sleep can play a significant role in maintaining a healthy weight and improving quality of life.
Integrating Physical Activity for a Leaner Waistline
Engaging in regular physical activity is paramount in the fight against aging-related belly fat. Exercise not only helps to maintain muscle mass but also aids in regulating fat cell production. Both aerobic and strength training exercises are beneficial for promoting lean body composition, improving metabolic rate, and reducing visceral fat accumulation.
Incorporating a variety of physical activities into your routine can make it easier to adhere to an active lifestyle. Whether it’s walking, swimming, or resistance training, finding enjoyable forms of exercise can significantly impact abdominal fat management and overall health as we age.
Frequently Asked Questions
What are the main causes of belly fat as we age?
Belly fat increases with age primarily due to changes in fat cell production, particularly from aging stem cells known as adipocyte progenitor cells (APCs). These cells become more active in older individuals, leading to a greater accumulation of fat around the abdomen. Additionally, lifestyle factors like stress and poor sleep can exacerbate these changes, contributing to weight gain with age.
How can I prevent belly fat from developing with age?
To prevent belly fat as you age, focus on three key strategies: prioritize protein intake to maintain muscle mass, optimize sleep and manage stress to lower cortisol levels, and limit ultraprocessed carbohydrates and refined sugars to reduce fat accumulation. These habits can help combat the effects of aging on fat storage and promote healthy aging.
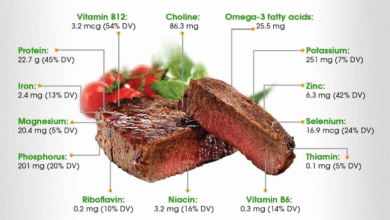
What is the importance of protein in preventing belly fat?
Protein plays a crucial role in preventing belly fat, especially as we age. Consuming 20 to 30 grams of protein at breakfast can help maintain lean muscle mass, which is essential for boosting metabolism and reducing fat cell production, particularly in the abdominal area. Foods such as Greek yogurt, eggs, and protein shakes are excellent options to incorporate into your diet.
How does stress affect belly fat accumulation?
Chronic stress significantly impacts belly fat accumulation by raising cortisol levels, a hormone linked to fat storage around the abdomen. Managing stress through practices like mindfulness and adequate sleep can help regulate cortisol and prevent weight gain with age.
Why is reducing ultraprocessed carbs important for preventing belly fat?
Reducing ultraprocessed carbohydrates and refined sugars is vital for preventing belly fat because these foods can lead to increased insulin resistance and promote fat accumulation, particularly visceral fat. Since aging adipose tissue behaves differently and is more prone to dysfunction, minimizing these types of foods can help regulate fat storage and support overall metabolic health.
| Key Points | Details |
|---|---|
| Why Belly Fat Increases with Age | Aging leads to increased fat cell production due to changes in stem cells and factors like stress and poor sleep. |
| Role of Adipocyte Progenitor Cells (APCs) | Older stem cells (APCs) are more likely to produce new fat cells, contributing to weight gain. |
| Signaling Pathway Involvement | The leukemia inhibitory factor receptor (LIFR) is linked to the creation of new fat cells in older individuals. |
| 3 Ways to Prevent Belly Fat | 1. **Prioritize Protein**: Start the day with 20-30g of protein to maintain muscle mass and stabilize blood sugar. 2. **Optimize Sleep and Stress**: Aim for 7-9 hours of quality sleep and manage stress to minimize fat storage. 3. **Limit Ultraprecessed Carbs**: Reduce intake of added sugars and processed carbs to decrease fat accumulation. |
Summary
To prevent belly fat, it is important to recognize that aging increases the risk of fat accumulation. By prioritizing protein intake, optimizing sleep and stress management, and limiting ultraprocessed carbohydrates and sugars, individuals can combat these age-related changes. Implementing these strategies can help maintain a healthy waistline and improve overall metabolic health.