Lung Cancer: Risks for Non-Smokers and Key Insights
Lung cancer is a formidable health concern, ranking as the second most prevalent cancer in the United States, affecting both smokers and non-smokers alike. While smoking is a well-known contributor to lung cancer risk factors, statistics reveal that up to 20% of lung cancers are diagnosed in individuals who have never smoked, highlighting the need for awareness about non-smoker lung cancer. Symptoms such as persistent cough, chest pain, and unintended weight loss often go unnoticed, stress the importance of lung cancer screening for early detection. With ongoing research into lung cancer prevention strategies, understanding modifiable risks from environmental factors and genetics is more critical than ever. Embracing awareness and education can empower individuals in their fight against lung cancer, potentially saving lives in the process.
Carcinoma of the lungs poses a significant threat, often stemming from a combination of genetic vulnerabilities and environmental exposures. Despite common perceptions, the disease does not discriminate, manifesting in those who have never engaged in tobacco use. Increased recognition of the disease’s prevalence among those without a traditional smoking history underscores the importance of focusing on lung health. Contemporary efforts aim to identify and mitigate lung cancer risk factors, such as pollution and secondhand smoke, while emphasizing proactive lung cancer screening to catch diseases early. As we delve into this topic, a comprehensive understanding of associated symptoms and effective prevention techniques will be essential for combating this widespread condition.
Understanding Lung Cancer in Non-Smokers
Lung cancer is often associated with smoking, yet a significant number of cases occur in non-smokers, highlighting a critical gap in public awareness. Researchers estimate that about 20% of lung cancer patients have never smoked or have smoked fewer than 100 cigarettes, underscoring the fact that lung cancer risk factors range beyond just tobacco use. Increased incidence rates among non-smokers have raised questions about the environmental and genetic factors that could contribute to lung cancer, urging a need for better education regarding symptoms and risk assessments.
This growing segment of lung cancer patients includes women and younger individuals, particularly those of Asian descent, as noted by experts in the field. As we explore the epidemiology of lung cancer, it’s essential to focus not only on smoking history but also on unexplored environmental factors such as air quality and secondhand smoke, which are increasingly recognized as vital contributors to lung carcinogenesis in never-smokers. Addressing these issues means developing comprehensive cancer prevention strategies that consider the unique risks faced by this population.
Key Lung Cancer Risk Factors
Understanding lung cancer risk factors is crucial for prevention and early detection. While smoking remains the most well-known cause of lung cancer, other factors, including exposure to environmental pollutants, need to be recognized as significant contributors. Studies indicate that radon exposure, occupational hazards involving asbestos or diesel exhaust, and even ambient air pollution can increase lung cancer risk, particularly among those who have never smoked. Recognizing these risk factors allows for more tailored prevention strategies that can help reduce the overall burden of lung cancer.
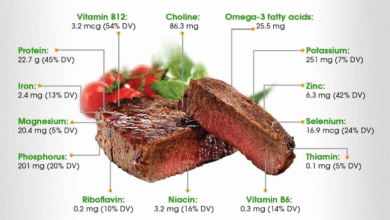
Moreover, lifestyle choices, such as poor diet and physical inactivity, can contribute to chronic inflammation, a key mechanism in cancer development. Both environmental and lifestyle factors underscore the complexity of lung cancer’s etiology. It is important to educate individuals about modifiable risk factors so they can implement changes that may lower their overall risk of developing lung cancer, irrespective of their smoking status. Comprehensive cancer prevention strategies must involve public health initiatives that focus on reducing exposure to harmful environmental agents.
Recognizing Lung Cancer Symptoms Early
Early detection of lung cancer significantly improves outcomes, yet recognizing the symptoms can often be challenging. Common signs such as persistent cough, unexplained weight loss, and chest pain may be overlooked or misattributed to other conditions, especially in non-smokers who may not suspect lung cancer. This expounds on the urgent need for awareness campaigns that stress the importance of early symptom recognition. It is essential for individuals, particularly non-smokers, to pay close attention to symptoms that deviate from their normal health patterns.
Furthermore, respiratory symptoms like wheezing or shortness of breath should not be dismissed, particularly if they linger or worsen over time. Individuals with a family history of lung cancer or other genetic predispositions should be especially vigilant. Understanding the unique manifestations of lung cancer symptoms in non-smokers can potentially lead to earlier diagnoses, significantly impacting survival rates. This highlights the need for healthcare providers to conduct thorough evaluations for anyone presenting with respiratory issues, regardless of their smoking history.
The Importance of Lung Cancer Screening
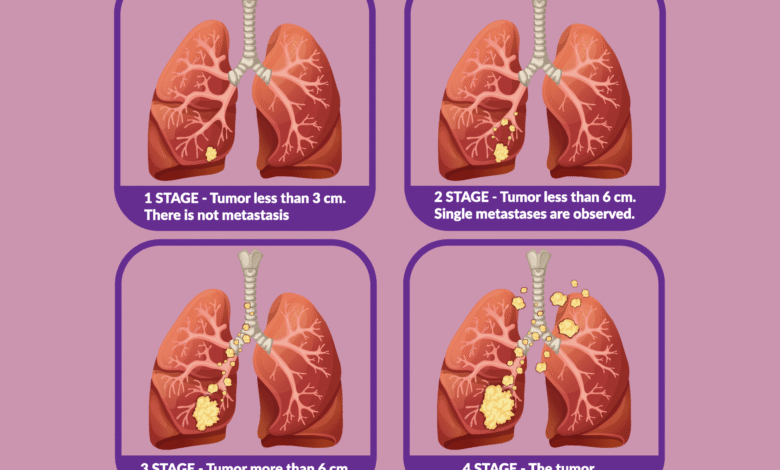
Current guidelines for lung cancer screening primarily focus on high-risk populations, specifically those with a significant smoking history, which leads to the exclusion of many non-smokers who may also be at risk. Traditional screening strategies utilizing low-dose CT scans are vital for early detection but often overlook individuals without a smoking background, despite emerging evidence that suggests an increasing number of lung cancer cases among this group. Broader screening parameters could bridge this gap, ensuring that more at-risk individuals receive appropriate surveillance.
As the understanding of lung cancer continues to evolve, conversations about the inclusion of non-smoking risk factors in screening protocols are becoming more prevalent. Experts advocate for further research to explore the relationships between screening efficacy and the unique demographic of lung cancer patients who have never smoked. By redefining who should be considered at risk, the healthcare community can enhance early detection strategies, improving survival outcomes and addressing the complexities of lung cancer in non-smokers.
Preventing Lung Cancer: Lifestyle Changes
Prevention is a critical component in the fight against lung cancer, and it begins with recognizing modifiable lifestyle factors. Although it might be impossible to entirely eliminate exposure to environmental risks, making conscious lifestyle changes can significantly reduce one’s risk of developing lung cancer. Individuals are encouraged to adopt a balanced diet rich in antioxidants, maintain a healthy weight, and engage in regular physical activity to strengthen their overall health, thereby potentially lowering the likelihood of inflammation-related cancers.
Additionally, staying informed about indoor air quality and minimizing exposure to known carcinogens such as asbestos and radon can further aid in lung cancer prevention. Understanding the significance of secondhand smoke can also empower individuals to advocate for cleaner environments, both at home and in public spaces. With a coherent focus on lifestyle modifications and environmental awareness, individuals can take proactive steps towards lowering their lung cancer risk.
The Role of Genetics in Lung Cancer
Genetic factors play a substantial role in determining an individual’s susceptibility to lung cancer, with research suggesting that around 8% of cases may arise due to inherited genetic predispositions. Understanding these genetic risk factors is crucial as they can inform targeted screening and prevention strategies tailored for individuals with a family history of lung cancer. This specificity is particularly important for younger patients who may not fit the traditional profile of a lung cancer patient but could still carry genetic mutations that predispose them to this disease.
Furthermore, identifying specific genetic mutations linked to lung cancer in non-smokers can illuminate differences in tumor biology between smokers and never-smokers. These distinctions are essential for developing personalized treatment plans that can improve outcomes. As research continues to evolve in this area, integrating genetic testing into routine evaluations for lung cancer risk could revolutionize early detection and prevention strategies, creating a more nuanced understanding of this complex disease.
Current Screening Guidelines and Controversies
The existing guidelines for lung cancer screening recommend annual low-dose CT scans for those aged 50 to 80 years with significant smoking histories, which raises important questions about inclusivity. As the rise of lung cancer cases among non-smokers continues to grow, experts urge a reevaluation of screening criteria that could potentially encompass people with known risk factors outside of smoking. Evidence indicating the need for broader guidelines is accumulating, reflecting a need for adapting healthcare practices to fit the changing demographics of lung cancer patients.
On the other hand, expanding screening eligibility presents its own set of challenges, including concerns over overdiagnosis and the psychological impact of false-positive results. With up to 50% of chest CT scans revealing benign pulmonary nodules, distinguishing between benign and malignant findings is crucial to effective patient management. Ongoing innovations in imaging and diagnostic tools hold promise for improving screening accuracy and minimizing the risks associated with overdiagnosis, paving the way for more effective lung cancer management.
Environmental Factors and Lung Cancer
Environmental factors play an increasingly recognized role in the development of lung cancer, particularly among non-smokers. pollutants in the air we breathe, exposure to hazardous materials at work, and even household chemicals can contribute to lung inflammation, which is known to facilitate cancer development. Recognizing and mitigating these risks is essential for reducing the incidence of lung cancer and enhancing public health initiatives. Addressing environmental pollutants can lead to substantial improvements in population health and cancer prevention.
Additionally, legislative measures aimed at controlling air quality and setting stricter regulations concerning hazardous substances in the workplace can significantly impact lung cancer rates. Increased public awareness regarding environmental risks, coupled with strong policy initiatives, could decrease exposure to known carcinogens and ultimately save lives. As we move forward, focusing on pollution and occupational safety will be integral to comprehensive lung cancer prevention strategies.
Understanding the Types of Lung Cancer
Lung cancer is classified primarily into two major types: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC accounts for approximately 80-85% of all lung cancer cases, embodying various subtypes including adenocarcinoma—a type frequently diagnosed in non-smokers. This distinction is crucial not only for treatment purposes but also for understanding the demographics of lung cancer patients and the broadening scope of lung cancer beyond traditional associations with smoking.
On the other hand, SCLC is more aggressive and has a poorer prognosis, thus necessitating different therapeutic strategies. The rise in non-small cell lung cancer among non-smokers suggests a paradigm shift in lung cancer epidemiology. Understanding these underlying differences could inform better-targeted therapies and result in improved outcomes for patients, particularly for those who previously might not have been screened due to their non-smoking status.
Frequently Asked Questions
What are the main risk factors for non-smoker lung cancer?
Non-smoker lung cancer risk factors include ambient air pollution, secondhand smoke, thoracic radiation exposure, and occupational hazards like radon and asbestos. Lifestyle factors, such as poor diet and lack of exercise, may also contribute to lung cancer risk among non-smokers.
What symptoms are commonly associated with lung cancer?
Common lung cancer symptoms include a persistent cough, chest pain, shortness of breath, wheezing, coughing up blood, and unexplained weight loss. It’s important to consult a healthcare provider if experiencing these symptoms, especially if you have risk factors for lung cancer.
How can lung cancer screening benefit non-smokers?
While current guidelines recommend lung cancer screening mainly for high-risk individuals with a smoking history, there is growing interest in including non-smokers with risk factors. Advances in imaging technology may help detect early-stage lung cancer, potentially improving outcomes.
What measures can be taken for lung cancer prevention?
Lung cancer prevention strategies include avoiding tobacco smoke, reducing exposure to air pollution, maintaining a healthy lifestyle with regular exercise and a balanced diet, and ensuring adequate ventilation in homes to reduce indoor pollutants. Early detection also plays a role in prevention.
Are there specific genetic factors associated with lung cancer in non-smokers?
Yes, approximately 8% of lung cancer cases are linked to inherited genetic predispositions. Having a family history of lung cancer can double an individual’s risk, and lung cancer in non-smokers may be associated with unique genetic mutations.
What is the current stance on lung cancer screening for non-smokers?
As of now, the U.S. Preventive Services Task Force does not recommend routine lung cancer screening for non-smokers due to the balance of risks and benefits. However, ongoing research may influence future guidelines to include non-smokers with significant risk factors.
What are the differences between non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC)?
Non-small cell lung cancer (NSCLC) comprises about 80-85% of lung cancers and includes types like adenocarcinoma and squamous cell carcinoma, commonly affecting non-smokers. Small cell lung cancer (SCLC) is more aggressive, spreads quickly, and is less common, representing a smaller percentage of lung cancers.
How does lifestyle affect lung cancer risk in non-smokers?
Lifestyle factors, such as poor diet, inactivity, and exposure to indoor pollutants, can increase lung cancer risk in non-smokers. Incorporating regular physical activity and a healthy diet can potentially provide a modest protective effect against lung cancer.
What is the role of environmental factors in lung cancer development for non-smokers?
Environmental factors such as air pollution and exposure to toxins like radon and asbestos significantly contribute to lung cancer risk in non-smokers. Inflammation caused by these pollutants may heighten the risk of developing lung cancer.
What should individuals with a family history of lung cancer do?
Individuals with a family history of lung cancer should discuss their risk with a healthcare provider. Genetic counseling and possibly genetic testing may be recommended to understand personal risk levels and to consider appropriate screening options.
| Key Points |
|---|
| Lung cancer is the second most common cancer in the U.S., with up to 20% of cases occurring in non-smokers. |
| Most lung cancers are classified as either non-small cell lung cancer (NSCLC) – which constitutes 80-85% of cases – or small cell lung cancer (SCLC). |
| Risk factors for non-smokers include air pollution, secondhand smoke, thoracic radiation, and occupational hazards. |
| Genetic predisposition plays a role in lung cancer, with about 8% of cases being inherited. |
| Screening recommendations currently focus on high-risk individuals, primarily heavy smokers, though interest is growing in including non-smokers. |
| New technologies and strategies are being developed to improve lung cancer detection and reduce overdiagnosis. |
Summary
Lung cancer remains a significant health challenge, affecting both smokers and non-smokers alike. As the second most common cancer in the U.S., the increasing diagnoses among non-smokers underscore the need for awareness of environmental and genetic risk factors. While lung cancer screening is primarily recommended for high-risk individuals with a history of smoking, evolving guidelines may soon account for the rising proportion of cases in non-smokers. Efforts to enhance early detection and reduce the harmful impacts of mistaken diagnoses are critical in the fight against this deadly disease.